- Record: found
- Abstract: found
- Article: found
Cardiac resynchronisation therapy in paediatric and congenital heart disease: differential effects in various anatomical and functional substrates
Read this article at
Abstract
Background:
Cardiac resynchronisation therapy (CRT) is increasingly used in children in a variety of anatomical and pathophysiological conditions, but published data are scarce.
Objective:
To record current practice and results of CRT in paediatric and congenital heart disease.
Patients:
One hundred and nine patients aged 0.24–73.8 (median 16.9) years with structural congenital heart disease (n = 87), congenital atrioventricular block (n = 12) and dilated cardiomyopathy (n = 10) with systemic left (n = 69), right (n = 36) or single (n = 4) ventricular dysfunction and ventricular dyssynchrony during sinus rhythm (n = 25) or associated with pacing (n = 84).
Main outcome measures:
Functional improvement and echocardiographic change in systemic ventricular function.
Results:
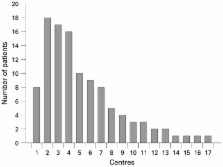
The z score of the systemic ventricular end-diastolic dimension decreased by median 1.1 (p<0.001). Ejection fraction (EF) or fractional area of change increased by a mean (SD) of 11.5 (14.3)% (p<0.001) and New York Heart Association (NYHA) class improved by median 1.0 grade (p<0.001). Non-response to CRT (18.5%) was multivariably predicted by the presence of primary dilated cardiomyopathy (p = 0.002) and poor NYHA class (p = 0.003). Presence of a systemic left ventricle was the strongest multivariable predictor of improvement in EF/fractional area of change (p<0.001). Results were independent of the number of patients treated in each contributing centre.
Related collections
Most cited references19
- Record: found
- Abstract: found
- Article: not found
Dual-chamber pacing or ventricular backup pacing in patients with an implantable defibrillator: the Dual Chamber and VVI Implantable Defibrillator (DAVID) Trial.
- Record: found
- Abstract: found
- Article: not found