- Record: found
- Abstract: found
- Article: found
Incidence and risk factors for oxygen desaturation during recovery from modified electroconvulsive therapy: A prospective observational study
Read this article at
Abstract
Background and Aims:
Electroconvulsive therapy (ECT) is an established modality of treatment for severe psychiatric illnesses. Among the various complications associated with ECT, oxygen desaturation is often under reported. None of the previous studies has evaluated the predictive factors for oxygen desaturation during ECT. The objective of this study was to evaluate the incidence of oxygen desaturation during recovery from anesthesia for modified ECT and evaluate its risk factors in a large sample.
Materials and Methods:
All patients aged above 15 years who were prescribed a modified ECT for their psychiatric illness over 1 year were prospectively included in this observational study. The association between age, body mass index (BMI), doses of thiopentone and suxamethonium, stimulus current, ECT session number, pre- and post-ECT heart rate and mean arterial pressure, seizure duration, and pre- and post ECT oxygen saturation, was systematically studied.
Results:
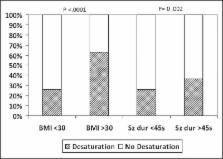
The incidence of oxygen desaturation was 29% (93/316 patients). Seizure duration and BMI were found to be significantly correlated with post ECT desaturation.
Conclusion:
In this prospective observational study, the incidence of oxygen desaturation during recovery from anesthesia for ECT was high. The study identified obesity and duration of seizure as the independent predictors of this complication. This knowledge is likely to help in identifying and optimizing such patients before subsequent ECT sessions.
Related collections
Most cited references18
- Record: found
- Abstract: found
- Article: not found
The impact of obesity on oxygen desaturation during sleep-disordered breathing.
- Record: found
- Abstract: found
- Article: not found
Life-threatening clozapine-induced gastrointestinal hypomotility: an analysis of 102 cases.
- Record: found
- Abstract: not found
- Article: not found