- Record: found
- Abstract: found
- Article: found
Spinal cord stimulation in chronic pain: evidence and theory for mechanisms of action
Read this article at
Abstract
Well-established in the field of bioelectronic medicine, Spinal Cord Stimulation (SCS) offers an implantable, non-pharmacologic treatment for patients with intractable chronic pain conditions. Chronic pain is a widely heterogenous syndrome with regard to both pathophysiology and the resultant phenotype. Despite advances in our understanding of SCS-mediated antinociception, there still exists limited evidence clarifying the pathways recruited when patterned electric pulses are applied to the epidural space. The rapid clinical implementation of novel SCS methods including burst, high frequency and dorsal root ganglion SCS has provided the clinician with multiple options to treat refractory chronic pain. While compelling evidence for safety and efficacy exists in support of these novel paradigms, our understanding of their mechanisms of action (MOA) dramatically lags behind clinical data. In this review, we reconstruct the available basic science and clinical literature that offers support for mechanisms of both paresthesia spinal cord stimulation (P-SCS) and paresthesia-free spinal cord stimulation (PF-SCS). While P-SCS has been heavily examined since its inception, PF-SCS paradigms have recently been clinically approved with the support of limited preclinical research. Thus, wide knowledge gaps exist between their clinical efficacy and MOA. To close this gap, many rich investigative avenues for both P-SCS and PF-SCS are underway, which will further open the door for paradigm optimization, adjunctive therapies and new indications for SCS. As our understanding of these mechanisms evolves, clinicians will be empowered with the possibility of improving patient care using SCS to selectively target specific pathophysiological processes in chronic pain.
Related collections
Most cited references277
- Record: found
- Abstract: not found
- Article: not found
Different immune cells mediate mechanical pain hypersensitivity in male and female mice.
- Record: found
- Abstract: found
- Article: not found
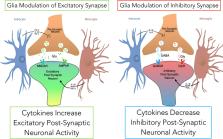
Tripartite synapses: glia, the unacknowledged partner.
- Record: found
- Abstract: found
- Article: not found