- Record: found
- Abstract: found
- Article: found
Clusters of Sudden Unexplained Death Associated with the Mushroom, Trogia venenata, in Rural Yunnan Province, China
Read this article at
Abstract
Introduction
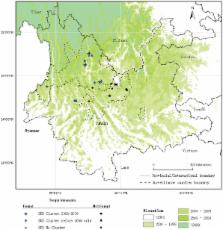
Since the late 1970's, time-space clusters of sudden unexplained death (SUD) in northwest Yunnan, China have alarmed the public and health authorities. From 2006–2009, we initiated enhanced surveillance for SUD to identify a cause, and we warned villagers to avoid eating unfamiliar mushrooms.
Methods
We established surveillance for SUD, defined as follows: sudden onset of serious, unexplained physical impairment followed by death in <24 hours. A mild case was onset of any illness in a member of the family or close socially related group of a SUD victim within 1 week of a SUD. We interviewed witnesses of SUD and mild case-persons to identify exposures to potentially toxic substances. We tested blood from mild cases, villagers, and for standard biochemical, enzyme, and electrolyte markers of disease.
Results
We identified 33 SUD, a 73% decline from 2002–2005, distributed among 21 villages of 11 counties. We found a previously undescribed mushroom, Trogia venenata, was eaten by 5 of 7 families with SUD clusters compared to 0 of 31 other control-families from the same villages. In T. venenata–exposed persons SUD was characterized by sudden loss of consciousness during normal activities. This mushroom grew nearby 75% of 61 villages that had time-space SUD clusters from 1975 to 2009 compared to 17% of 18 villages with only single SUD (p<0.001, Fisher's exact test).
Related collections
Most cited references31
- Record: found
- Abstract: found
- Article: not found
Arrhythmogenic marker for the sudden unexplained death syndrome in Thai men.
- Record: found
- Abstract: found
- Article: not found
New electrocardiographic leads and the procainamide test for the detection of the Brugada sign in sudden unexplained death syndrome survivors and their relatives.
- Record: found
- Abstract: found
- Article: not found