- Record: found
- Abstract: found
- Article: found
Diamidines versus Monoamidines as Anti- Pneumocystis Agents: An in vivo Study
research-article
Dimitri Stanicki
1 ,
Muriel Pottier
2 ,
Nausicaa Gantois
2 ,
Claire Pinçon
3 ,
Delphine Forge
1 ,
Isabelle Mahieu
4 ,
Sébastien Boutry
4 ,
Jean Jacques Vanden Eynde
1
,
* ,
Anna Martinez
2 ,
Eduardo Dei-Cas
2
,
5 ,
El-Moukhtar Aliouat
2
01 July 2013
Read this article at
There is no author summary for this article yet. Authors can add summaries to their articles on ScienceOpen to make them more accessible to a non-specialist audience.
Abstract
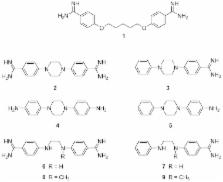
Some compounds articulated around a piperazine or an ethylenediamine linker have been evaluated in vitro to determine their activity in the presence of a 3T6 fibroblast cell line and an axenic culture of Pneumocystis carinii, respectively. The most efficient antifungal derivatives, namely N, N′-bis(benzamidine-4-yl)ethane-1,2-diamine (compound 6, a diamidine) and N-(benzamidine-4-yl)- N′-phenylethane-1,2-diamine (compound 7, a monoamidine), exhibited no cytotoxicity and were evaluated in vivo in a rat model. Only the diamidine 6 emerged as a promising hit for further studies.
Related collections
Most cited references37
- Record: found
- Abstract: found
- Article: not found
Update on the diagnosis and treatment of Pneumocystis pneumonia.
Eva Carmona, Andrew Limper (2011)
- Record: found
- Abstract: found
- Article: not found
Pneumocystis infection in humans: diagnosis and treatment.
Lindsay Calderon, Isabelle Joly, Sonia Gutierrez … (2010)