- Record: found
- Abstract: found
- Article: found
Residential location of people with chronic spinal cord injury: the importance of local health care infrastructure
Read this article at
Abstract
Background
People with spinal cord injury (SCI) suffer from complex secondary health conditions and rely on specialized health care services, which are often centralized and difficult to reach for individuals living in remote areas. As a consequence, they might move to regions where they expect better access to care. The aims of this study were: 1) to identify regions where people with SCI live compared with the general population, 2) to examine whether their choice of residence is related to the availability of local health care infrastructure, and 3) to ascertain determinants of their consideration to change residence when aging.
Methods
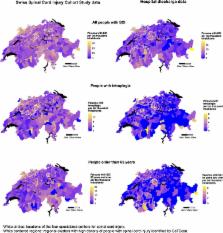
This study used information from a nationwide Swiss SCI cohort and inpatient hospital discharge data. To detect clusters in the distribution of people with chronic SCI in Switzerland, a spatial cluster detection test was conducted using the normative population of a region as offset. To identify associations between the residential location of people with SCI and infrastructure variables, a negative binomial model was set up at a regional level with the frequency of people with SCI as outcome, geographical indicators as explanatory variables, and the normative population as offset. Determinants of the consideration to change residence when aging were investigated using logistic regression models.
Results
People with SCI were not living equally distributed among the normative population, but clustered in specific areas. They were more likely than the general population to reside close to specialized SCI centers, in areas with a high density of outpatient physicians, and in urban regions. People with SCI living in rural areas were more likely to consider relocating when aging than those living in urban areas. However, only a few people with SCI considered moving closer to specialized centers when such a move required crossing language barriers.
Related collections
Most cited references28
- Record: found
- Abstract: found
- Article: not found
Traveling towards disease: transportation barriers to health care access.
- Record: found
- Abstract: found
- Article: not found
Utilization of health services following spinal cord injury: a 6-year follow-up study.
- Record: found
- Abstract: found
- Article: not found