- Record: found
- Abstract: found
- Article: found
Renal blood flow in sepsis
Read this article at
Abstract
Introduction
To assess changes in renal blood flow (RBF) in human and experimental sepsis, and to identify determinants of RBF.
Method
Using specific search terms we systematically interrogated two electronic reference libraries to identify experimental and human studies of sepsis and septic acute renal failure in which RBF was measured. In the retrieved studies, we assessed the influence of various factors on RBF during sepsis using statistical methods.
Results
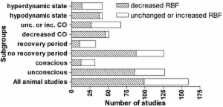
We found no human studies in which RBF was measured with suitably accurate direct methods. Where it was measured in humans with sepsis, however, RBF was increased compared with normal. Of the 159 animal studies identified, 99 reported decreased RBF and 60 reported unchanged or increased RBF. The size of animal, technique of measurement, duration of measurement, method of induction of sepsis, and fluid administration had no effect on RBF. In contrast, on univariate analysis, state of consciousness of animals ( P = 0.005), recovery after surgery ( P < 0.001), haemodynamic pattern (hypodynamic or hyperdynamic state; P < 0.001) and cardiac output ( P < 0.001) influenced RBF. However, multivariate analysis showed that only cardiac output remained an independent determinant of RBF ( P < 0.001).
Conclusion
The impact of sepsis on RBF in humans is unknown. In experimental sepsis, RBF was reported to be decreased in two-thirds of studies (62 %) and unchanged or increased in one-third (38%). On univariate analysis, several factors not directly related to sepsis appear to influence RBF. However, multivariate analysis suggests that cardiac output has a dominant effect on RBF during sepsis, such that, in the presence of a decreased cardiac output, RBF is typically decreased, whereas in the presence of a preserved or increased cardiac output RBF is typically maintained or increased.
Related collections
Most cited references193
- Record: found
- Abstract: found
- Article: not found
The natural history of the systemic inflammatory response syndrome (SIRS). A prospective study.
- Record: found
- Abstract: found
- Article: not found
Hospital-acquired renal insufficiency: a prospective study.
- Record: found
- Abstract: not found
- Article: not found