- Record: found
- Abstract: found
- Article: found
Clinical outcome of cardiac resynchronization therapy in dilated-phase hypertrophic cardiomyopathy

Read this article at
Abstract
Backgrounds
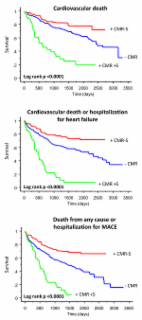
Clinical trials have demonstrated that cardiac resynchronization therapy (CRT) is effective in patients with “non-ischemic cardiomyopathy”. However, patients with dilated-phase hypertrophic cardiomyopathy (DHCM) have been generally excluded from such trials. We aimed to compare the clinical outcome of CRT in patients with DHCM, idiopathic dilated cardiomyopathy (IDCM), or ischemic cardiomyopathy (ICM).
Methods
A total of 312 consecutive patients (DHCM: n = 16; IDCM: n = 231; ICM: n = 65) undergoing CRT in Fuwai hospital were studied respectively. Response to CRT was defined as reduction in left ventricular end-systolic volume (LVESV) ≥ 15% at 6-month follow-up.
Results
Compared with DHCM, IDCM was associated with a lower total mortality (HR: 0.35, 95% CI: 0.13–0.90), cardiac mortality (HR: 0.29; 95% CI: 0.11–0.77), and total mortality or heart failure (HF) hospitalizations (HR: 0.34, 95% CI: 0.17–0.69), independent of known confounders. Compared with DHCM, the total mortality, cardiac mortality and total mortality or HF hospitalizations favored ICM but were not statistically significant (HR: 0.59, 95% CI: 0.22–1.61; HR: 0.59, 95% CI: 0.21–1.63; HR: 0.54, 95% CI: 0.26–1.15; respectively). Response rate to CRT was lower in the DHCM group than the other two groups although the differences didn't reach statistical significance.
Related collections
Most cited references15
- Record: found
- Abstract: not found
- Article: not found
2010 Focused Update of ESC Guidelines on device therapy in heart failure: an update of the 2008 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure and the 2007 ESC guidelines for cardiac and resynchronization therapy. Developed with the special contribution of the Heart Failure Association and the European Heart Rhythm Association.
- Record: found
- Abstract: found
- Article: found
Cardiac resynchronization therapy guided by late gadolinium-enhancement cardiovascular magnetic resonance

- Record: found
- Abstract: found
- Article: found