- Record: found
- Abstract: found
- Article: found
Digital innovation evaluation: user perceptions of innovation readiness, digital confidence, innovation adoption, user experience and behaviour change
Abstract
Background
Innovation spread is a key policy objective for health systems world-wide, but adoption success varies enormously. We have developed a set of short generic user-reported measures to help understand how and why healthcare innovations spread. This work builds on the literature and on practical experience in developing and using patient-reported outcome measures.
Measures
The Innovation Readiness Score measures user perceptions of how much they are open to and up-to-date with new ideas, and whether their organisations are receptive to and capable of innovation. It is based on Rogers’ classification of innovativeness (innovator, early adopter, early majority, etc).
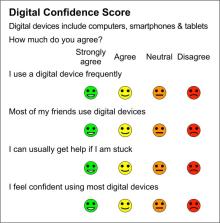
The Digital Confidence Score rates users’ digital literacy and confidence to use digital products, with dimensions of familiarity, social pressure, support and digital self-efficacy.
The Innovation Adoption Score rates the adoption process in terms of coherence and reflective thought before, during and after implementation. It is based on Normalisation Process Theory.
The User Satisfaction measure assesses a digital product in terms of usefulness, ease of use, support and satisfaction.
The Behaviour Change measure covers user perceptions of their capability, opportunity and motivation to change behaviour, based on the COM-B model.
These measures have been mapped onto Greenhalgh’s NASSS Framework (non-adoption, abandonment and challenges to scale-up, spread and sustainability of health and care technologies).
Related collections
Most cited references6
- Record: found
- Abstract: found
- Article: not found
Assessment of Remote Heart Rhythm Sampling Using the AliveCor Heart Monitor to Screen for Atrial Fibrillation

- Record: found
- Abstract: found
- Article: found
Analysing the role of complexity in explaining the fortunes of technology programmes: empirical application of the NASSS framework

- Record: found
- Abstract: found
- Article: found