- Record: found
- Abstract: found
- Article: found
Therapeutic Use of Mesenchymal Stem Cell-Derived Exosomes: From Basic Science to Clinics
Read this article at
Abstract
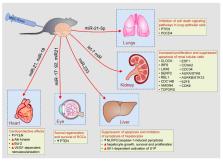
Mesenchymal stem cells (MSC) are, due to their immunosuppressive and regenerative properties, used as new therapeutic agents in cell-based therapy of inflammatory and degenerative diseases. A large number of experimental and clinical studies revealed that most of MSC-mediated beneficial effects were attributed to the effects of MSC-sourced exosomes (MSC-Exos). MSC-Exos are nano-sized extracellular vesicles that contain MSC-derived bioactive molecules (messenger RNA (mRNA), microRNAs (miRNAs)), enzymes, cytokines, chemokines, and growth factors) that modulate phenotype, function and homing of immune cells, and regulate survival and proliferation of parenchymal cells. In this review article, we emphasized current knowledge about molecular and cellular mechanisms that were responsible for MSC-Exos-based beneficial effects in experimental models and clinical trials. Additionally, we elaborated on the challenges of conventional MSC-Exos administration and proposed the use of new bioengineering and cellular modification techniques which could enhance therapeutic effects of MSC-Exos in alleviation of inflammatory and degenerative diseases.
Related collections
Most cited references43

- Record: found
- Abstract: found
- Article: found
Mesenchymal Stem Cell-Derived Exosomes and Other Extracellular Vesicles as New Remedies in the Therapy of Inflammatory Diseases

- Record: found
- Abstract: found
- Article: found
Exosome Mediated Delivery of miR-124 Promotes Neurogenesis after Ischemia

- Record: found
- Abstract: found
- Article: found