- Record: found
- Abstract: found
- Article: found
Stigma and Attitudes toward Patients with Psychiatric Illness among Postgraduate Indian Physicians

Read this article at
Abstract
Background:
Due to paucity of psychiatrists in India, psychiatric patients often present to other doctors. We aimed to study nonpsychiatric residents’ attitude and stigma toward psychiatric patients.
Methods:
A total of 57 postgraduate trainees participated in a cross-sectional study in a tertiary hospital in New Delhi. Attitudes to psychiatric patients were assessed using the attitude to mental illness questionnaire (AMIQ) and the perceived stigma questionnaire. This was correlated with sociodemographic information.
Results:
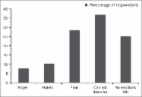
Over 70% residents accepted mentally ill patients as friends and felt they were equally employable. However, AMIQ demonstrated a negative attitude towards patients with schizophrenia. Perceived competence in dealing with psychiatric patients was associated with adequate undergraduate exposure (Chi-square = 7.270, P = 0.026) and correlated with positive attitudes ( t-test, P = 0.0008).
Related collections
Most cited references6

- Record: found
- Abstract: found
- Article: found
Myths, beliefs and perceptions about mental disorders and health-seeking behavior in Delhi, India

- Record: found
- Abstract: found
- Article: found
Training and National deficit of psychiatrists in India – A critical analysis
- Record: found
- Abstract: found
- Article: found