- Record: found
- Abstract: found
- Article: found
Treatment planning study of the 3D dosimetric differences between Co-60 and Ir-192 sources in high dose rate (HDR) brachytherapy for cervix cancer
Read this article at
Abstract
Purpose
To evaluate whether Co-60 is equivalent to Ir-192 for HDR cervical brachytherapy, through 3D-DVH dose comparisons in standard and optimised plans. Previous studies have only considered 2D dosimetry, point dose comparisons or identical loading. Typical treatment times and economics are considered.
Material and methods
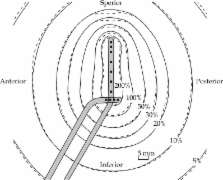
Plans were produced for eight cervix patients using Co-60 and Ir-192 sources, CT imaging and IU/two-channel-ring applicator (Eckert Ziegler BEBIG). The comparison was made under two conditions: (A) identical dwell positions and loading, prescribed to Point A and (B) optimised source dwells, prescribed to HR-CTV. This provided a direct comparison of inherent differences and residual differences under typical clinical plan optimisation. The DVH (target and OAR), ICRU reference points and isodose distributions were compared. Typical treatment times and source replacement costs were compared.
Results
Small differences ( p < 0.01) in 3D dosimetry exist when using Co-60 compared to Ir-192, prescribed to Point A with identical loading patterns, particularly 3.3% increase in rectum D2cc. No significant difference was observed in this parameter when prescribing to the HR-CTV using dwell-time optimisation. There was no statistically significant difference in D90 between the two isotopes. Co-60 plans delivered consistently higher V150% (mean +4.4%, p = 0.03) and V400% (mean +11.6%, p < 0.01) compared to Ir-192 in optimised plans. Differences in physical source properties were overwhelmed by geometric effects.
Conclusions
Co-60 may be used as an effective alternative to Ir-192 for HDR cervix brachytherapy, producing similar plans of equivalent D90, but with logistical benefits. There is a small dose increase along the extension of the source axis when using Co-60 compared to Ir-192, leading to small rectal dose increases for identical loading patterns. This can be eliminated by planning optimisation techniques. Such optimisation may also be associated with increases in the overdose volume (V150-V400) with Co-60 compared to Ir-192.
Related collections
Most cited references23

- Record: found
- Abstract: found
- Article: found
Dysphagia in head and neck cancer patients following intensity modulated radiotherapy (IMRT)
- Record: found
- Abstract: found
- Article: not found
Technical note: Dosimetric study of a new Co-60 source used in brachytherapy.
- Record: found
- Abstract: not found
- Article: not found