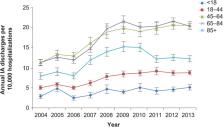
The epidemiology of Clostridium difficile infection (CDI) has been shifting over the past decade. Since 2000, the molecular evolution of the hypervirulent toxigenic bacterial strain BI/NAP1/027, which causes severe disease in massive outbreak settings, has been well documented ( 1 – 4 ). Furthermore, the increasing detection of this strain in the United States and other countries coincides with reports of increasing hospitalizations either resulting from or complicated by CDI and associated with increased case-fatality rates ( 5 – 7 ). Although in the past it was not thought to affect pediatric populations substantially, CDI has more recently been implicated as an increasingly prevalent diarrheal pathogen in children ( 8 – 10 ). Moreover, evidence suggests that a large proportion of pediatric CDI cases are community-acquired infections and that many of these infections lack the traditional risk factor of exposure to antimicrobial drugs ( 11 – 13 ). These changes in the epidemiology of pediatric CDI, although not definitively caused by the BI/NAP1/027 strain, are likely related to this strain because at least 2 reports suggest a high prevalence (10%–38%) of this strain in pediatric CDI populations and a 4× increase in complication rates associated with this strain compared with other strains ( 14 , 15 ). Current age-specific epidemiology of CDI among children remains poorly studied. Literature predating the emergence of the epidemic strain suggests that although up to 67% of all neonates (i.e., 1 data source potentially indicates a higher chance of accuracy. In addition, the format in which we analyzed 1 of the databases (Kids’ Inpatient Database [KID]) did not enable separating newborn discharges (defined as those hospitalizations during which the child was born) from those of other children 55 years on a maternal record, and mixed neonatal and maternal records), i.e., no chart reviews are undertaken by the agency. For the current study, all data were derived in aggregate from the publicly available HCUPNet website ( 18 ). Because the years for which data were available were 1997, 2000, 2003, and 2006, our observations were limited to these periods. We examined the annual incidence of CDI-related hospitalizations on the basis of the International Classification of Diseases, 9th revision, clinical modification (ICD-9-CM), code 008.45 (intestinal infection with C. difficile) as a proportion of all hospitalizations. We additionally determined the time trends for CDI as the principal discharge diagnosis in this population. Finally, to understand better the context of increasing CDI-related hospitalizations, we examined trends in hospitalizations related to other diarrheal diseases, specifically Salmonella (ICD-9-CM 00.30), rotavirus (ICD-9-CM 008.61), viral enteritis (ICD-9-CM 008.8), and other infectious enteritides (ICD-9-CM codes 009.0–009.3, 487.8). The second analysis was a cross-sectional characterization of all CDI hospitalizations for patients 80% of all hospitalized children <1 year of age in the HCUP and KID databases. We could not determine whether the relatively high rate of CDI-related hospitalizations among non-newborn infants represents predominantly true disease or colonization. Although more specific than recovery of a toxin-producing strain from culture, even the detection of free toxins A, B, or both in the stool of a symptomatic infant does not ensure a pathogenic role for C. difficile, especially if another cause for diarrhea can be identified. Rates of hospitalizations for rotavirus infections have exhibited a similar increase as those with CDI between 1997 and 2006. Although 2 recent analyses of discharge data for adults suggest that non-CDI causes of diarrhea are not likely leading to a reporting bias as the explanation for the observed increase in CDI rates ( 22 , 23 ), the situation may be different for children in whom rotavirus is a serious pathogen and related hospitalizations are clearly increasing. Although Kim et al. did not report an increase in the frequency of testing for C. difficile in their study, our findings implicate this finding as a distinct possibility that needs to be investigated further ( 9 ). Our study has several limitations. First, case identification was based on administrative coding, thus predisposing to misclassification. However, the degree of misclassification may not be substantial because multiple studies have shown the ICD-9-CM code 008.45 to be a relatively accurate way to identify CDI ( 24 – 26 ). Second, because we had no clinical data available, we could not distinguish stool colonization from CDI infection. Third, we were unable to distinguish community-acquired from healthcare-associated disease. However, our study has several strengths. Because we explored 2 databases and discovered results that are highly consistent not only with each other but with those of previous recent investigations, we have augmented the accuracy of estimates of pediatric CDI incidence ( 9 ). In addition, our data are generalizable to most US-based institutions that care for the pediatric populations. This generalizability sets our results apart from those reported previously because they were limited to the highly specialized setting of children’s hospitals ( 8 , 9 , 11 ). In summary, the incidence of CDI in the pediatric population appears to be increasing in US hospitals. A reporting bias for diarrheal diseases may play a role in this trend given the concomitant increase in rotavirus-related hospitalizations we identified. Future data may clarify this finding because widespread immunization with available rotavirus vaccines may soon lead to reduced incidence of related hospitalizations. The low incidence of CDI-related hospitalizations among newborns reflects current recommendations against routine testing and may support the concept that C. difficile does not cause disease among neonates. In contrast, the relatively high rate of CDI-related hospitalizations among non-newborn infants indicates an urgent need for studies to determine how often C. difficile causes true disease in this population.