- Record: found
- Abstract: found
- Article: not found
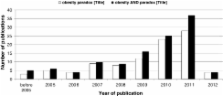
The obesity paradox in chronic disease: facts and numbers
Read this article at
Abstract
Body size, particularly large, is a matter of concern among the lay public. Whether this is justified depends upon the state of health and should be judged individually. For patients with established chronic disease, there is sufficient evidence to support the benefits of large body size, i.e., the obesity paradox. This uniform finding is shared over a variety of cardiovascular, pulmonary, and renal diseases and is counterintuitive to the current concepts on ideal body weight. The scientific community has to increase the awareness about differences for optimal body size in health and disease. Simultaneously, clinicians have to be aware about body weight dynamics implications and should interpret the changes in the context of an underlying disease in order to implement the best available management.
Related collections
Most cited references18
- Record: found
- Abstract: found
- Article: not found
Overweight, obesity, and mortality in a large prospective cohort of persons 50 to 71 years old.
- Record: found
- Abstract: found
- Article: not found
The obesity paradox: body mass index and outcomes in patients with heart failure.
- Record: found
- Abstract: found
- Article: not found
