- Record: found
- Abstract: found
- Article: found
Clinical Presentation and Outcome of Sinonasal Tumors in a Nigerian Tertiary Hospital – 6-year Review
Read this article at
Abstract
Background:
Sinonasal tumor is an uncommon tumor in Nigeria, but the burden of the disease in terms of morbidity and mortality is on the increase. The aim of this study is to evaluate the pattern of presentation and outcome of sinonasal tumor in our center.
Methodology:
This was a retrospective review of all the patients with sinonasal cancer seen in Ear, Nose, and Throat Department of the hospital between January 2008 and December 2013. The patients' biodata, clinical presentation, stage of the disease at presentation, identifiable risk factors, histopathological findings, and outcome were presented.
Results:
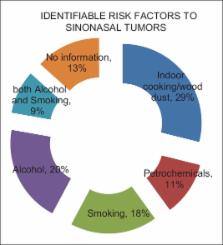
A total of 22 patients were diagnosed with sinonasal cancer out of 71 patients (31%) with head/neck cancers during the period of study. There were 12 males (54.5%) and 10 females (45.5%) with a mean age of 51 ± 2.1 years. Epistaxis, nasal blockage, and discharge were seen in all patients though 41% of patients presented first to the ophthalmologist due to proptosis. Identifiable risk factors were exposure to wood dust (29%) and petrochemical products in (11%). Most patients presented first at advanced stages of the disease (82%). Histologically, well-differentiated squamous cell carcinoma was the most common (54.6%) followed by nonintestinal well-differentiated adenocarcinoma in 18.2% and plasmacytoma (9.1%). Chemoradiation was the mainstay of management in (38%) though 13.6% had total maxillectomy with postsurgical chemoradiation and 50.4% defaulted due to cost of management.
Conclusion:
Health education on early presentation and efforts at early detection of the disease are needed to achieve cure. Exposure to the identifiable risk factors should be reduced by protective measures. Easy access to radiotherapy at affordable price will surely improve the outcome of this disease.
Related collections
Most cited references19
- Record: found
- Abstract: found
- Article: not found
Craniofacial resection for malignant paranasal sinus tumors: Report of an International Collaborative Study.
- Record: found
- Abstract: found
- Article: not found