- Record: found
- Abstract: found
- Article: found
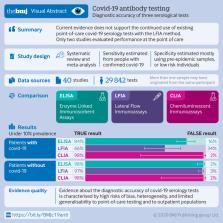
Diagnostic accuracy of serological tests for covid-19: systematic review and meta-analysis
Read this article at
Abstract
Objective
To determine the diagnostic accuracy of serological tests for coronavirus disease-2019 (covid-19).
Data sources
Medline, bioRxiv, and medRxiv from 1 January to 30 April 2020, using subject headings or subheadings combined with text words for the concepts of covid-19 and serological tests for covid-19.
Eligibility criteria and data analysis
Eligible studies measured sensitivity or specificity, or both of a covid-19 serological test compared with a reference standard of viral culture or reverse transcriptase polymerase chain reaction. Studies were excluded with fewer than five participants or samples. Risk of bias was assessed using quality assessment of diagnostic accuracy studies 2 (QUADAS-2). Pooled sensitivity and specificity were estimated using random effects bivariate meta-analyses.
Main outcome measures
The primary outcome was overall sensitivity and specificity, stratified by method of serological testing (enzyme linked immunosorbent assays (ELISAs), lateral flow immunoassays (LFIAs), or chemiluminescent immunoassays (CLIAs)) and immunoglobulin class (IgG, IgM, or both). Secondary outcomes were stratum specific sensitivity and specificity within subgroups defined by study or participant characteristics, including time since symptom onset.
Results
5016 references were identified and 40 studies included. 49 risk of bias assessments were carried out (one for each population and method evaluated). High risk of patient selection bias was found in 98% (48/49) of assessments and high or unclear risk of bias from performance or interpretation of the serological test in 73% (36/49). Only 10% (4/40) of studies included outpatients. Only two studies evaluated tests at the point of care. For each method of testing, pooled sensitivity and specificity were not associated with the immunoglobulin class measured. The pooled sensitivity of ELISAs measuring IgG or IgM was 84.3% (95% confidence interval 75.6% to 90.9%), of LFIAs was 66.0% (49.3% to 79.3%), and of CLIAs was 97.8% (46.2% to 100%). In all analyses, pooled sensitivity was lower for LFIAs, the potential point-of-care method. Pooled specificities ranged from 96.6% to 99.7%. Of the samples used for estimating specificity, 83% (10 465/12 547) were from populations tested before the epidemic or not suspected of having covid-19. Among LFIAs, pooled sensitivity of commercial kits (65.0%, 49.0% to 78.2%) was lower than that of non-commercial tests (88.2%, 83.6% to 91.3%). Heterogeneity was seen in all analyses. Sensitivity was higher at least three weeks after symptom onset (ranging from 69.9% to 98.9%) compared with within the first week (from 13.4% to 50.3%).
Related collections
Most cited references49
- Record: found
- Abstract: found
- Article: not found
Temporal profiles of viral load in posterior oropharyngeal saliva samples and serum antibody responses during infection by SARS-CoV-2: an observational cohort study
- Record: found
- Abstract: found
- Article: not found
Antibody responses to SARS-CoV-2 in patients of novel coronavirus disease 2019

- Record: found
- Abstract: found
- Article: found