- Record: found
- Abstract: found
- Article: found
Social inequalities in multimorbidity, frailty, disability, and transitions to mortality: a 24-year follow-up of the Whitehall II cohort study
Summary
Background
Social inequalities in mortality persist in high-income countries with universal health care, and the mechanisms by which these inequalities are generated remain unclear. We aimed to examine whether social inequalities were present before or after the onset of adverse health conditions (multimorbidity, frailty, and disability).
Methods
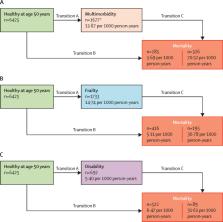
Our analysis was based on data from the ongoing Whitehall II cohort study, which enrolled British civil servants aged 35–55 years in 1985–88. Participants were assessed for three indicators of socioeconomic status (education, occupational position, and literacy) at age 50 years. Participants underwent clinical examinations (in 2002–04, 2007–09, 2012–13, and 2015–16) for assessment of frailty (two or more of low physical activity, slow walking speed, poor grip strength, weight loss, and exhaustion) and disability (two or more difficulties in bathing, dressing, going to the toilet, transferring, feeding, and walking). In addition, electronic health records were used to assess the incidence of multimorbidity (two or more of diabetes, coronary heart disease, stroke, chronic obstructive pulmonary disease, depression, arthritis, cancer, dementia, and Parkinson's disease) and mortality. In analyses adjusted for sociodemographic factors, we used multistate models to examine social inequalities in transitions from healthy state to adverse health conditions and subsequently to mortality.
Findings
Of 10 308 individuals in the Whitehall II study cohort, 6425 had relevant data available at 50 years and to the end of follow-up on Aug 31, 2017, and were included in our analysis. Participants were followed up for a median of 23·6 years (IQR 19·6–28·9). 1694 (26·4%) of 6425 participants developed multimorbidity, 1733 (27·0%) became frail, 692 (10·8%) had a disability, and 611 (9·5%) died. Multimorbidity (hazard ratio [HR] 4·12 [95% CI 3·41–4·98]), frailty (HR 2·38 [95% CI 1·93–2·93]), and disability (HR 1·73 [95% CI 1·34–2·22]) were associated with increased risk of mortality; these associations were not modified by socioeconomic status. In multistate models, occupation was the socioeconomic status indicator that was most strongly associated with inequalities in the transition from healthy state to multimorbidity (HR 1·54 [95% CI 1·37–1·73]), to frailty (HR 2·08 [95% CI 1·85–2·33]), and to disability (HR 1·44 [95% CI 1·18–1·74]). Socioeconomic status indicators did not affect transitions to mortality in those with multimorbidity, frailty, or disability.
Interpretation
Socioeconomic status affects the risk of multimorbidity, frailty, and disability, but does not affect the risk of mortality after the onset of these adverse health conditions. Therefore, primary prevention is key to reducing social inequalities in mortality. Of the three adverse health conditions, multimorbidity had the strongest association with mortality, making it a central target for improving population health.
Related collections
Most cited references28
- Record: found
- Abstract: found
- Article: found
Frailty in elderly people
- Record: found
- Abstract: found
- Article: not found