- Record: found
- Abstract: found
- Article: found
Effects of probenecid and cimetidine on the pharmacokinetics of nemonoxacin in healthy Chinese volunteers
Abstract
Purpose
To investigate the effects of probenecid and cimetidine on the pharmacokinetics of nemonoxacin in humans.
Methods
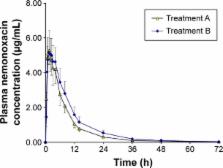
Two independent, open-label, randomized, crossover studies were conducted in 24 (12 per study) healthy Chinese volunteers. In Study 1, each volunteer received a single oral dose of 500 mg of nemonoxacin alone or with 1.5 g of probenecid divided into three doses within 25 hours. In Study 2, each volunteer received a single oral dose of 500 mg of nemonoxacin alone or with multiple doses of cimetidine (400 mg thrice daily for 7 days). The plasma and urine nemonoxacin concentrations were determined using validated liquid chromatography–tandem mass spectrometry methods.
Results
Coadministration of nemonoxacin with probenecid reduced the renal clearance (CL r) of nemonoxacin by 22.6%, and increased the area under the plasma concentration–time curve from time 0 to infinity (AUC 0−∞) by 26.2%. Coadministration of nemonoxacin with cimetidine reduced the CL r of nemonoxacin by 13.3% and increased AUC 0−∞ by 9.4%. Coadministration of nemonoxacin with probenecid or cimetidine did not significantly affect the maximum concentration of nemonoxacin or the percentage of the administered dose recovered in the urine.
Most cited references19
- Record: found
- Abstract: found
- Article: not found
The clinical pharmacokinetics of levofloxacin.
- Record: found
- Abstract: found
- Article: not found
Efficacy and safety of nemonoxacin versus levofloxacin for community-acquired pneumonia.
- Record: found
- Abstract: found
- Article: not found