- Record: found
- Abstract: found
- Article: found
Comparing endobronchial ultrasound-guided fine needle aspiration specimens with and without rapid on-site evaluation
letter

31 January 2012
Read this article at
There is no author summary for this article yet. Authors can add summaries to their articles on ScienceOpen to make them more accessible to a non-specialist audience.
Abstract
Sir,
We read with great interest the recent article by Carruth-Griffin et al. entitled
“Utility of on-site evaluation of endobronchial ultrasound-guided transbronchial needle
aspiration specimens”[1] and commend the authors on a well-written paper, which addresses
an important and timely topic of interest to cytologists evaluating these specimens.
We would like to share our institution's experience as it relates to the use of rapid
on-site evaluation (ROSE) in the clinical decision-making process for endobronchial
ultrasound-guided fine needle aspiration (EBUS-FNA) cases, because our experience
has been different and likely reflects different institutional practices.
With regard to clinical decision making at the time of ROSE, the impact of the ROSE
may depend on who is performing the FNA. The authors of this recent study state that
the EBUS-FNAs were performed mainly by clinicians/bronchoscopists in their Interventional
Pulmonary Department.[1] In this setting, the patients are usually under conscious
sedation in a bronchoscopy suite, and cannot have an immediate surgical intervention
performed regardless of the ROSE. In our institution, the majority of the EBUS-FNA
procedures are performed under general anesthesia in the operating room by thoracic
surgeons. This is advantageous in that it allows for the patient to proceed to mediastinoscopy
if the findings at the time of ROSE are benign or indeterminate, while sparing those
patients with malignancy from having a more invasive procedure. The surgeons at our
institution rely on the ROSE and preliminary diagnosis to help with their intraprocedural
clinical decision making on whether or not to convert to a mediastinoscopy, which
is similar to the use of intraoperative frozen section. The decision-making algorithm
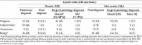
used at our institution is summarized in
Figure 1 and has been previously published by our clinical colleagues.[2]
Figure 1
Clinical decision-making algorithm for patients with suspicious mediastinal lymphadenopathy
utilizing EBUS-FNA (FDG = Fluorodeoxyglucose, PET = Positron emission tomography,
ROSE = Rapid on-site evaluation)
The paper also states that the diagnostic yield does not differ in cases with or without
ROSE. However, in our experience, the use of ROSE allows one to evaluate for adequacy
and to triage the material appropriately, which is particularly important for cases
with a suspected malignancy where ancillary studies, including immunostains, flow
cytometry, and/or molecular studies are extremely important.[3] Being present at the
time of ROSE allows the cytologist to request additional material when needed and
to allocate dedicated passes for cell block to enrich the cellularity, once a diagnosis
can be reached. For instance, when present at the EBUS-FNA, if the first pass shows
metastatic carcinoma, then any additional material from other passes can be used to
make a cell block. However, in the absence of ROSE, the clinicians may use valuable
material to make additional unnecessary slides, which could compromise the cell block
yield and lead to the inability to perform ancillary studies, if these are to be performed
on the cell block. Table 5 in the paper by Carruth-Griffin A et al.[1] points out
that the number of cases with cell block preparation was slightly higher in the subset
of cases with ROSE (92% vs 88%) and that more of the cases with ROSE had immunostains
performed (29% vs 15%), special stains performed (9% vs 3%), and flow cytometry performed
(11% vs 0.6%). Furthermore, the authors point out that although there was a similar
percent of malignant cases in the cases with and without ROSE, immunostains were utilized
more in those cases with ROSE (63% vs 37%), as was flow cytometry (94% vs 6%). The
increased use of ancillary studies in the group with ROSE may reflect a better diagnostic
yield of material for ancillary studies, in comparison with the group without ROSE.
This is an important point because of the increasing need to perform molecular testing
on non-small-cell carcinomas of the lung, which have predictive and prognostic value,
and are becoming increasingly more important for the management of these patients.
Given that cytological specimens are criticized for not having sufficient material
for these important tests, we have found that being present to appropriately allocate
sufficient material in EBUS-FNA cases for the aforementioned tests is important at
our institution. After all, establishing a diagnosis of malignancy is just one aspect
of what we are being asked to provide in today's era of personalized medicine. If
we are unable to go further and perform crucial ancillary studies and molecular tests,
then we are not optimizing the EBUS-FNA procedure and we are potentially subjecting
a patient to additional diagnostic procedures, which increases healthcare costs and
decreases the quality of care for a patient.[4]
In conclusion, the utility of ROSE in EBUS-FNAs may differ based on who is performing
the procedure (clinician/bronchoscopist vs thoracic surgeon) and the different treatment
algorithms employed in different institutions. This is important as many institutions
are now trying to establish their own protocols for dealing with these new cytological
specimens, which will likely increase over time as more minimally invasive approaches
replace more invasive and costly surgical procedures. In our EBUS-FNA experience,
if there is a potential for following the procedure with surgery, such as mediastinoscopy,
then the use of ROSE with a preliminary diagnosis can be crucial for appropriate patient
care and has a similar role as frozen section evaluation. As the results of this informative
article point out, perhaps each institution should critically analyze their own practice
to determine how best to use ROSE in EBUS-FNAs.
Related collections
Most cited references4
- Record: found
- Abstract: found
- Article: found
Utility of on-site evaluation of endobronchial ultrasound-guided transbronchial needle aspiration specimens
Adrienne Griffin, Lauren Schwartz, Zubair Baloch (2011)

- Record: found
- Abstract: found
- Article: found
Diagnostic difficulties and pitfalls in rapid on-site evaluation of endobronchial ultrasound guided fine needle aspiration
- Record: found
- Abstract: not found
- Article: not found
Seize the opportunity: underutilization of fine-needle aspiration biopsy to inform targeted cancer therapy decisions.
Michael Clark (2009)