- Record: found
- Abstract: found
- Article: found
Resistance and the management of complicated skin and skin structure infections: the role of ceftobiprole
Abstract
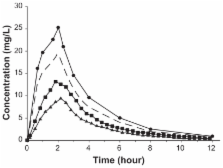
Antimicrobial resistant bacteria are an increasing concern due to the resulting increase in morbidity, mortality, and health-care costs associated with the administration of inadequate or delayed antimicrobial therapy. The implications of inadequate antimicrobial therapy in complicated skin and skin structure infections (cSSSIs) have gained more attention recently, most likely due to the recent emergence of community-acquired methicillin resistant Staphylococcus aureus (MRSA) and the already high prevalence of MRSA in the nosocomial setting. Due to the continuous threat of resistance arising and the limitations of currently available agents for the treatment of cSSSIs, it is necessary to develop new antimicrobials for this indication. Ceftobiprole medocaril, the prodrug of ceftobiprole, is a parental investigational cephalosporin for the treatment of cSSSIs displaying a wide-spectrum of activity against both Gram-positive and Gram-negative species, including MRSA. Ceftobiprole displays noncomplex linear pharmacokinetics, is eliminated primarily by glomerular filtration, and distributes to extracellular fluid. Additionally, it has been shown that the extent of distribution to the site of action with regard to cSSSIs, ie, the extracellular space fluid of subcutaneous adipose tissue and skeletal muscle, is expected to be efficacious, as free concentrations meet efficacy targets for most pathogens. Similar to other beta-lactams, it displays an excellent safety and tolerability profile with the primary adverse events being dysgeusia in healthy volunteers, resulting from the conversion of the prodrug to the active, and nausea in patients. Ceftobiprole has demonstrated noninferiority in two large-scale pivotal studies comparing it to vancomycin, clinical cure rates 93.3% vs 93.5%, respectively, or vancomycin plus ceftazidime, clinical cure rates 90.5% vs 90.2%, respectively. Given the pharmacokinetic and pharmacodynamic properties, ceftobiprole is a promising new agent for the treatment of cSSSIs and has the potential to be used as a single agent for empiric treatment.