- Record: found
- Abstract: found
- Article: found
Three-dimensional and thermal surface imaging produces reliable measures of joint shape and temperature: a potential tool for quantifying arthritis
Read this article at
Abstract
Introduction
The assessment of joints with active arthritis is a core component of widely used outcome measures. However, substantial variability exists within and across examiners in assessment of these active joint counts. Swelling and temperature changes, two qualities estimated during active joint counts, are amenable to quantification using noncontact digital imaging technologies. We sought to explore the ability of three dimensional (3D) and thermal imaging to reliably measure joint shape and temperature.
Methods
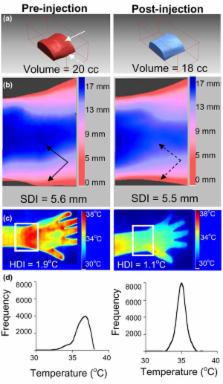
A Minolta 910 Vivid non-contact 3D laser scanner and a Meditherm med2000 Pro Infrared camera were used to create digital representations of wrist and metacarpalphalangeal (MCP) joints. Specialized software generated 3 quantitative measures for each joint region: 1) Volume; 2) Surface Distribution Index (SDI), a marker of joint shape representing the standard deviation of vertical distances from points on the skin surface to a fixed reference plane; 3) Heat Distribution Index (HDI), representing the standard error of temperatures. Seven wrists and 6 MCP regions from 5 subjects with arthritis were used to develop and validate 3D image acquisition and processing techniques. HDI values from 18 wrist and 9 MCP regions were obtained from 17 patients with active arthritis and compared to data from 10 wrist and MCP regions from 5 controls. Standard deviation (SD), coefficient of variation (CV), and intraclass correlation coefficients (ICC) were calculated for each quantitative measure to establish their reliability. CVs for volume and SDI were <1.3% and ICCs were greater than 0.99.
Results
Thermal measures were less reliable than 3D measures. However, significant differences were observed between control and arthritis HDI values. Two case studies of arthritic joints demonstrated quantifiable changes in swelling and temperature corresponding with changes in symptoms and physical exam findings.
Related collections
Most cited references38
- Record: found
- Abstract: found
- Article: not found
The meaning and use of the area under a receiver operating characteristic (ROC) curve.
- Record: found
- Abstract: found
- Article: not found
The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis.
- Record: found
- Abstract: found
- Article: not found