- Record: found
- Abstract: found
- Article: found
Dosimetric impact of point A definition on high-dose-rate brachytherapy for cervical cancer: evaluations on conventional point A and MRI-guided, conformal plans
Read this article at
Abstract
Purpose
To investigate the dosimetric impact of point A definitions on both conventional point A plans and MRI-guided conformal high-dose-rate (HDR) brachytherapy plans.
Material and methods
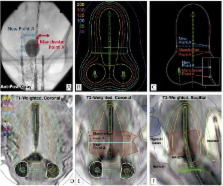
Fifty-five HDR plans of 36 patients with FIGO stage I to IV cervical cancer were retrospectively studied; these included 30 conventional treatments and 25 conformal plans. Two different point A definitions were explored: the revised Manchester point A and the new point A as recommended by the American Brachytherapy Society. Conventional plans were produced by varying only the point A definition and the normalized isodose lines. Conformal plans were retrospectively generated per GEC-ESTRO recommendations based upon 3.0 Tesla MRI data.
Results
Small yet significant variations were found in point A locations (mean: 0.5 cm, maximum: 2.1 cm, p < 0.001). The use of a new point A caused minimal dose variation for both conventional and conformal plans. Conventional plans normalized to the new point A generated up to 12% (avg. 1-3%) higher overall dose in terms of higher total reference air kerma than plans normalized to other points. Dosimetric changes due to point A definitions were up to 11-12% (avg. less than 2%) on target volumes or organs-at-risk.
Related collections
Most cited references21
- Record: found
- Abstract: found
- Article: not found
American Brachytherapy Society consensus guidelines for locally advanced carcinoma of the cervix. Part I: general principles.
- Record: found
- Abstract: found
- Article: not found