- Record: found
- Abstract: found
- Article: not found
An analysis of the utilisation of chemoprophylaxis against Pneumocystis jirovecii pneumonia in patients with malignancy receiving corticosteroid therapy at a cancer hospital
Read this article at
Abstract
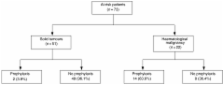
Pneumocystis jirovecii pneumonia (PCP) is associated with high mortality in immunocompromised patients without human immunodeficiency virus infection. However, chemoprophylaxis is highly effective. In patients with solid tumours or haematologic malignancy, several risk factors for developing PCP have been identified, predominantly corticosteroid therapy. The aims of this study were to identify the potentially preventable cases of PCP in patients receiving corticosteroid therapy at a tertiary care cancer centre and to estimate the frequency of utilisation of chemoprophylaxis in these patients. Two retrospective reviews were performed. Over a 10-year period, 14 cases of PCP were identified: no cases were attributable to failed chemoprophylaxis, drug allergy or intolerance. During a 6-month period, 73 patients received high-dose corticosteroid therapy (⩾25 mg prednisolone or ⩾4 mg dexamethasone daily) for ⩾4 weeks. Of these, 22 (30%) had haematologic malignancy, and 51 (70%) had solid tumours. Fewer patients with solid tumours received prophylaxis compared to patients with haematologic malignancy (3.9 vs 63.6%, P<0.0001). Guidelines for PCP chemoprophylaxis in patients with haematologic malignancy or solid tumours who receive corticosteroid therapy are proposed. Successful primary prevention of PCP in this population will require a multifaceted approach targeting the suboptimal prescribing patterns for chemoprophylaxis.
Related collections
Most cited references57
- Record: found
- Abstract: found
- Article: not found
Summary of the Guidelines for Preventing Opportunistic Infections among Hematopoietic Stem Cell Transplant Recipients.
- Record: found
- Abstract: found
- Article: not found
Results of treatment with hyper-CVAD, a dose-intensive regimen, in adult acute lymphocytic leukemia.
- Record: found
- Abstract: found
- Article: not found
