- Record: found
- Abstract: found
- Article: found
Effect of drug utilization reviews on the quality of in-hospital prescribing: a quasi-experimental study
Read this article at
Abstract
Background
Drug utilization review (DUR) programs are being conducted in Canadian hospitals with the aim of improving the appropriateness of prescriptions. However, there is little evidence of their effectiveness. The objective of this study was to assess the impact of both a retrospective and a concurrent DUR programs on the quality of in-hospital prescribing.
Methods
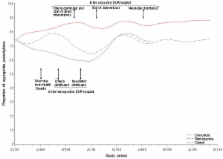
We conducted an interrupted time series quasi-experimental study. Using explicit criteria for quality of prescribing, the natural history of cisapride prescription was established retrospectively in three university-affiliated hospitals. A retrospective DUR was implemented in one of the hospitals, a concurrent DUR in another, whereas the third hospital served as a control. An archivist abstracted records of all patients who were prescribed cisapride during the observation period. The effect of DURs relative to the control hospital was determined by comparing estimated regression coefficients from the time series models and by testing the statistical significance using a 2-tailed Student's t test.
Related collections
Most cited references26
- Record: found
- Abstract: not found
- Book: not found
Exploratory data analysis.
- Record: found
- Abstract: found
- Article: not found
Principles of educational outreach ('academic detailing') to improve clinical decision making.
- Record: found
- Abstract: found
- Article: not found