- Record: found
- Abstract: found
- Article: found
Toxic Dilated Cardiomyopathy: Recognizing a Potentially Reversible Disease
case-report
Read this article at
There is no author summary for this article yet. Authors can add summaries to their articles on ScienceOpen to make them more accessible to a non-specialist audience.
Abstract
Introduction
The use of illicit drugs has increased in recent years
1
. Related to this increase, there is a growing need
to recognise and properly treat the adverse effects associated with the consumption
of these drugs.
These substances can induce several cardiovascular (CV) complications, being this
acute or chronic
1
. Some of them
are the ischemic and arrhythmic events, the development of dilated cardiomyopathy
(DCM) and the left ventricular systolic dysfunction (LVSD).
There are several types of drugs with different pharmacological and
pathophysiological properties, and synergism is described between them
1
. Among these, cocaine and heroin
stand out.
The key to a successful intervention towards one of these adverse effects is the high
index of suspicion and early intervention.
Case Report
We describe the case of a 46-year-old Portuguese woman, a heroin and cocaine addicted
(intra-venous consumption, as well smoking) since the age of 23, a chronic bearer
of
hepatitis B and C virus, with a previous history of pulmonary tuberculosis (treated)
and moderate drinking habits.
The patient was admitted to the Emergency Department (ED) with exertional dyspnea
of
four months' evolution and progressive worsening in the last month (dyspnea on mild
exertion). She denied chest pain, fever, chills or other associated symptoms. She
denied recent travelling outside Portugal. She was tachycardic (115 beats per
minute) and hypertensive (168/90 mmHg). In cardiac auscultation, she showed a
holosystolic murmur, grade II/VI, at the level of the mitral focus, with axillary
irradiation. She also showed signs of pulmonary congestion, hepatomegaly and mild
peripheral edemas.
The chest x-ray showed an increased cardiothoracic index, signs of vascular
cephalization, with hypotransparency at the level of the lower thirds of both lung
fields, compatible with pulmonary congestion. The electrocardiogram revealed sinus
tachycardia and left bundle branch block (LBBB). Analytically, she had normochromic
and normocytic anemia (hemoglobin of 11.9 g/dl), normal renal function and ionogram;
overall elevation of liver enzymes (AST 287 U/L, ALT 207 U/L, Gamma-GT of 109 U/L,
total bilirubin of 2.04 mg/dl, direct bilirubin of 0.4 mg/dL) as well as of BNP's
levels (3600 pg/ mL). She presented no significant elevation of myocardial necrosis
or inflammatory biomarkers. Computed tomography angiography excluded signs of
pulmonary thromboembolism and showed the presence of bilateral pleural effusion and
alveolar consolidation.
For additional assessment, the patient underwent an echocardiography, which showed
dilatation of the left cardiac chambers (left ventricular
[LV] end diastolic volume of 125 ml/ m2; maximal atrial
volume of 39 ml/m
2
), with global
and severe LVSD (ejection fraction [EF] of 11%), without asymmetries
in segmental contractility, and two small apical thrombi were identified (Figure 1).
Mild right ventricular dysfunction
was also evident.
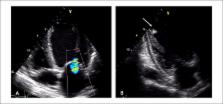
Figure 1
Transthoracic echocardiogram at admission showing the presence of dilated
cardiomyopathy, with mitral regurgitation due to poor coaptation of the
valve leaflets (A) and thrombus adhering to the apex (arrow) (B).
Given these findings, we conducted the diagnosis of decompensated heart failure (HF)
in a patient with dilated cardiomyopathy and ventricular dysfunction, with probable
toxic etiology.
She started pharmacological treatment of HF (loop diuretics, β blockers
[BB] and angiotensin-converting enzyme [ACE] inhibitor),
as well as anticoagulant, with favourable clinical evolution. She was discharged by
the 5thday of hospitalization, and she was oriented to the outpatient
Consultation in the hospital and to the Support Centre for Addicts. She remained in
functional class I of NYHA since the first month after discharge. After six months
of total abstinence from drugs, under optimized treatment for HF, she was completely
asymptomatic, with BNP values below 10 pg/ mL. The echocardiographic reassessment
showed normal cardiac chambers size and recovery of the biventricular systolic
function (LV end diastolic volume of 57 ml/m2; maximal atrial volume of
21 ml/m2; LV EF 62%), with no evidence of intracavitary thrombi. The oral
hypocoagulant was suspended, keeping up the therapy with BB (carvedilol) and the ACE
inhibitor (lisinopril).
Discussion
All the types of recreational drugs may induce important CV complications and they
are responsible for high morbidity and mortality.
Following the cannabinoids, the psychostimulant drugs are the most widely consumed
illicit substances. Acute intoxication by these drugs is a frequent cause of resort
to the ED, particularly for chest pain, as well as an important cause of drug
related death
2
.
Psychostimulants and opioids have been related with LVSD. However, few clinical
reports have illustrated the role of drug abstinence in the recovery of heart
failure and myocardial dysfunction, which can be achieved in a short period of
time
3,4
. The major cardiovascular manifestations, secondary
to cocaine and heroin drug abuse, will be reviewed here.
The CV toxicity associated with psychostimulants is well described and it is an
phenomenon independent from the consumption standard, dosage or administration
route.
CV effects of cocaine abuse derive essentially from the activation of the sympathetic
nervous system, contributing to the occurrence of arrhythmias and ischemic
events
3,5
.
The ischemic events are undoubtedly the more frequent CV complications in consumers
of stimulants such as cocaine
2
.
There is even a temporal relation between the consumption and the event. It was
found that two thirds of acute myocardial infarctions (AMI) related to the effect
of
cocaine occur within the first three hours after its consumption
6
.
Ischemia may result from the increased maximum oxygen consumption by the myocardium,
as well as from phenomena of coronary vasospasm, probably in relation to the
activation of α-adrenergic receptors in the coronary vessels
5
. In addition, cocaine promotes
thrombogenesis, by atherosclerotic plaque formation and platelet activation and
aggregation
3,7
.
More rarely, the chronic use of cocaine is associated with the development of DCM
and
LVSD, the latter being potentially reversible with a consumption
discontinuation
7
. The
mechanisms which cause the systolic dysfunction include direct toxic effects of
cocaine, the presence of sustained ischemia, the persistent hyperadrenergic state
and inflammatory mechanisms including the alteration of cytokine production and
induction of myocyte apoptosis
5
.
Opioids are another type of recreational drugs. Heroin is the most widely consumed
illicit opiate. They act by increasing parasympathetic activity and decreasing
sympathetic activity, which can cause bradycardia and hypotension
1
.
Like psychostimulants, this kind of drugs has also been associated with the
occurrence of several types of arrhythmias, ischemic events and potentially
reversible LVSD
1,3
. It is believed that the most likely mechanism of
myocardial ischemia is also vasospasm.
Moreover, acute heroin intoxication can cause noncardiogenic pulmonary edema due to
the disruption of alveolarcapillary membrane integrity.
The indicated treatment for the vast majority of patients admitted under recreational
drug use is the conventional treatment, considering its complications and supportive
measures. However, the approach to chest pain in patients consuming cocaine is still
somewhat controversial with relation to the use of BB, as it can exacerbate coronary
vasospasm in a more serious phase of acute coronary syndrome (ACS), by inhibiting
the vasodilatory effect inherent to the stimulation of α2adrenergic
receptors
8
. Although there
are not enough studies about the best therapeutic strategy in this clinical context,
current recommendations suggest that nitrates and calcium channel blockers are the
preferred drugs for the initial control of arterial hypertension, coronary
vasoconstriction and tachycardia (verapamil). In case of insufficient response to
this therapeutic strategy, it is reasonable to administer a β blocker with
additional α-blocking effect (for example, labetalol)
9
.
Conclusion
The consumption of recreational drugs can induce an extensive range of cardiovascular
manifestations, causing many serious medical conditions which include arrhythmias,
ischemic events and LVSD.
The case described significantly illustrates the importance of recognizing the toxic
etiology, particularly for recreational drug abuse, associated with dilated
cardiomyopathy, which when treated properly and with proof, is potentially
reversible and may have a favourable prognosis.
Related collections
Most cited references8
- Record: found
- Abstract: not found
- Article: not found
Cardiovascular complications of cocaine use.
Stephen Hillis, R. Lange (2001)
- Record: found
- Abstract: not found
- Article: not found
2011 ACCF/AHA Focused Update Incorporated Into the ACC/AHA 2007 Guidelines for the Management of Patients With Unstable Angina/Non-ST-Elevation Myocardial Infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines.
Jeffrey Anderson, Cynthia Adams, Elliott M. Antman … (2011)