- Record: found
- Abstract: found
- Article: found
Comparison of anti-anaerobic antimicrobial strategies in cancer patients with febrile neutropenia and gastrointestinal symptoms
Read this article at
Abstract
Background
The current study sought to compare 28-day mortality rates in cancer patients with febrile neutropenia (FN) and gastrointestinal (GI) symptoms who underwent monotherapy using an antibiotic with antipseudomonal and anti-anaerobic activity (piperacillin-tazobactam or a carbapenem) and a group treated with a combination of cefepime-metronidazole.
Findings
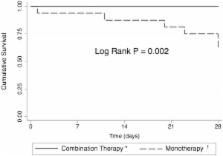
We performed a prospective cohort study in a single tertiary hospital from October 2009 to August 2011. All consecutive adult cancer patients admitted with FN secondary to intensive chemotherapy and GI symptoms (abdominal pain, diarrhea or perianal pain) were evaluated. Kaplan-Meier curves were used for calculating time-dependent occurence of death. In total, 37 patients with FN and GI symptoms were evaluated (15 in monotherapy arm and 22 in the combination therapy arm). Treatment with combination cefepime and metronidazole resulted in a lower 28-day mortality rate compared with piperacillin-tazobactam or carbapenem monotherapy (0% versus 40%; log-rank P=0.002).
Conclusions
Results of the present study suggest a significant reduction in mortality in cancer patients with FN and GI symptoms treated with combination cefepime-metronidazole therapy compared with monotherapy using agents with antipseudomonal and anti-anaerobic activity. Further randomized trials are warranted to confirm the superior results using combination therapy in patients with FN and GI symptoms.
Related collections
Most cited references14
- Record: found
- Abstract: found
- Article: not found
Clinical practice guideline for the use of antimicrobial agents in neutropenic patients with cancer: 2010 update by the infectious diseases society of america.
- Record: found
- Abstract: found
- Article: not found
The Multinational Association for Supportive Care in Cancer risk index: A multinational scoring system for identifying low-risk febrile neutropenic cancer patients.
- Record: found
- Abstract: found
- Article: not found