- Record: found
- Abstract: found
- Article: found
Solitaire Thrombectomy for Acute Stroke Due to Intracranial Atherosclerosis-Related Occlusion: ROSE ASSIST Study
Read this article at
Abstract
Background: Solitaire, a representative stent retriever, has shown high performance in removing embolic clots. However, its reperfusion potential in intracranial atherosclerotic stenosis (ICAS)-related occlusions has rarely been reported. In this ROSE ASSIST study, we hypothesized that Solitaire device is as effective and safe for removing in situ thrombi in ICAS-related occlusions as it is for removal of embolic occlusions.
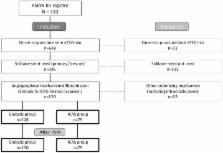
Methods: Data from ASIAN KR, an observational multicenter registry ( n = 720) enrolling patients who have undergone endovascular treatment for acute cervicocephalic artery occlusions, were retrospectively reviewed. Through blinded evaluations, occlusions were classified as ICAS-related (significant fixed focal stenosis observed at the occlusion site during endovascular treatment) or embolic (no or minimal stenosis observed). Among patients treated within 720 min after stroke onset, those who undertook Solitaire thrombectomy and whose underlying etiology was ICAS-related or embolic were included. The primary endpoint was immediate successful reperfusion (modified Treatment In Cerebral Ischemia 2b−3) after Solitaire stent retrieval. The safety endpoint included intracerebral hemorrhagic transformation and subarachnoid hemorrhage. Comparative analyses were performed between embolic and ICAS-related occlusions with 2:1 propensity score matching.
Results: In total, 303 patients (embolic, 228; ICAS-related, 75) were included in the analyses. As for the primary endpoint, the immediate successful reperfusion rate following Solitaire thrombectomy did not differ between the two etiologic groups after propensity score matching (73.1% embolic vs. 65.8% ICAS-related, p = 0.261). The final successful reperfusion grade was also similar in the two groups (79.3 vs. 72.0%, p = 0.219). The grades and frequencies of intracerebral hemorrhagic transformation and subarachnoid hemorrhage did not differ between groups ( p = 0.134 and p = 0.269, respectively).
Conclusions: The immediate reperfusion performance in terms of thrombus removal of Solitaire thrombectomy for ICAS-related occlusions was similar to that for embolic occlusions.
Related collections
Most cited references26
- Record: found
- Abstract: found
- Article: not found
Stenting versus aggressive medical therapy for intracranial arterial stenosis.
- Record: found
- Abstract: found
- Article: not found
A critical appraisal of propensity-score matching in the medical literature between 1996 and 2003.
- Record: found
- Abstract: found
- Article: not found