- Record: found
- Abstract: found
- Article: found
Comparison of the efficacy and safety of URSL, RPLU, and MPCNL for treatment of large upper impacted ureteral stones: a randomized controlled trial
Read this article at
Abstract
Background
There are three minimally invasive methods for the management of large upper impacted ureteral stones: mini-percutaneous nephrolithotomy (MPCNL), transurethral ureteroscope lithotripsy (URSL), and retroperitoneal laparoscopic ureterolithotomy (RPLU). This study aimed to compare MPCNL, URSL, and RPLU, and to evaluate which one is the best choice for large upper impacted ureteral stones.
Methods
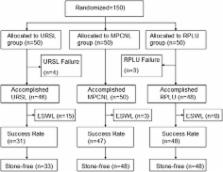
Between January 2012 and December 2015, at the Department of Urology, Huai’an First People’s Hospital, 150 consecutively enrolled patients with a large upper impacted ureteral stone (>15 mm) were included. The patients were randomly divided (1:1:1) into the MPCNL, URSL, and RPLU groups. The primary endpoint was success of stone removal measured 1 month postoperatively and the secondary endpoints were intraoperative and postoperative parameters and complications.
Results
Fifteen patients needed auxiliary ESWL after URSL, and 3 patients after MPCNL, but none after RPLU. The stone clearance rate was 96% (48/50) in the MPCNL group and 72% (33/46) in the URSL group. In the RPLU group the stones were completely removed and the stone clearance rate was 100% (48/48) ( P = 0.021 vs. URSL; P = 0.083 vs. MPCNL). Operation-related complications were similar among the three groups (all P > 0.05). Hospital stay was shorter in the URSL group compared with MPCNL ( P = 0.003). Operation time was the shortest with URSL and the longest with MPCNL (all P < 0.05).
Conclusions
MPCNL and RPUL are more suitable for upper ureteral impacted stones of >15 mm. URSL could be considered if the patient is not suitable for general anesthesia, or the patient requests transurethral uretroscopic surgery.
Trial registration
This study was registered with the Chinese Clinical Trial Registry (Registration number: ChiCTR-INR-17011507; Registration date: 2017–5-22).
Related collections
Most cited references19
- Record: found
- Abstract: found
- Article: not found
Changing gender prevalence of stone disease.
- Record: found
- Abstract: found
- Article: not found
