- Record: found
- Abstract: found
- Article: found
Association of MRI-derived radiomic biomarker with disease-free survival in patients with early-stage cervical cancer
Read this article at
Abstract
Pre-treatment survival prediction plays a key role in many diseases. We aimed to determine the prognostic value of pre-treatment Magnetic Resonance Imaging (MRI) based radiomic score for disease-free survival (DFS) in patients with early-stage (IB-IIA) cervical cancer.
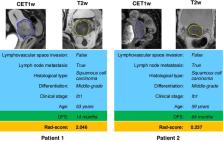
Methods: A total of 248 patients with early-stage cervical cancer underwent radical hysterectomy were included from two institutions between January 1, 2011 and December 31, 2017, whose MR imaging data, clinicopathological data and DFS data were collected. Patients data were randomly divided into the training cohort (n = 166) and the validation cohort (n=82). Radiomic features were extracted from the pre-treatment T2-weighted (T2w) and contrast-enhanced T1-weighted (CET1w) MR imagings for each patient. Least absolute shrinkage and selection operator (LASSO) regression and Cox proportional hazard model were applied to construct radiomic score (Rad-score). According to the cutoff of Rad-score, patients were divided into low- and high- risk groups. Pearson's correlation and Kaplan-Meier analysis were used to evaluate the association of Rad-score with DFS. A combined model incorporating Rad-score, lymph node metastasis (LNM) and lymphovascular space invasion (LVI) by multivariate Cox proportional hazard model was constructed to estimate DFS individually.
Results: Higher Rad-scores were significantly associated with worse DFS in the training and validation cohorts ( P<0.001 and P=0.011, respectively). The Rad-score demonstrated better prognostic performance in estimating DFS (C-index, 0.753; 95% CI: 0.696-0.805) than the clinicopathological features (C-index, 0.632; 95% CI: 0.567-0.700). However, the combined model showed no significant improvement (C-index, 0.714; 95%CI: 0.642-0.784).
Conclusion: The results demonstrated that MRI-derived Rad-score can be used as a prognostic biomarker for patients with early-stage (IB-IIA) cervical cancer, which can facilitate clinical decision-making.
Related collections
Most cited references29
- Record: found
- Abstract: not found
- Article: not found
Radiomics Analysis for Evaluation of Pathological Complete Response to Neoadjuvant Chemoradiotherapy in Locally Advanced Rectal Cancer
- Record: found
- Abstract: not found
- Article: not found
Radiomics of Multiparametric MRI for Pretreatment Prediction of Pathologic Complete Response to Neoadjuvant Chemotherapy in Breast Cancer: A Multicenter Study
- Record: found
- Abstract: not found
- Article: not found