- Record: found
- Abstract: found
- Article: found
JAHA Spotlight on Psychosocial Factors and Cardiovascular Disease
research-article
Read this article at
There is no author summary for this article yet. Authors can add summaries to their articles on ScienceOpen to make them more accessible to a non-specialist audience.
Abstract
Psychosocial factors, such as stress, adversity, socioeconomic status, depression,
and anxiety, are associated with overall health and with cardiovascular health in
particular. In this issue of the Journal of the American Heart Association (JAHA),
we have featured a group of articles that explore different aspects of the complex
relationships between psychosocial factors and cardiovascular health. Importantly,
psychosocial factors have different prevalence among different demographic groups,
and as such, may be key for addressing disparities in the development of cardiovascular
disease (CVD) and its morbidity and mortality.
Disparities in cardiovascular health between blacks and whites have existed for some
time. In this Spotlight, Tabb and colleagues used novel methods to explore spatial
heterogeneity in racial differences in cardiovascular health in the United States.1
They found that blacks consistently have worse cardiovascular health compared with
whites and that these racial differences exist across the nation, even after considering
residency in the Stroke Belt. These findings highlight the need for geographically
based interventions and policies to address disparities.
Stress can come in many forms. Heikkilä and colleagues evaluated job strain in nearly
140 000 patients with no previous hospitalization for peripheral artery disease and
found that job strain was associated with an increase in the risk of hospitalization
for the disease.2 Although stress has been associated with the development of myocardial
infarction and stroke, this study is novel because it demonstrates stress is also
associated with adverse peripheral artery disease outcomes. In another study, Glover
and colleagues evaluated the association between goal‐striving stress, the stress
from striving for goals, and CVD.3 Goal‐striving stress is a psychological phenomenon
related to striving for upward mobility and awareness of having little success and
may have affected blacks for decades. Using the JHS (Jackson Heart Study), they found
that a quarter of the study population had high levels of goal‐striving stress and
that among women, this was associated with a lower risk of stroke but a higher risk
of CVD.
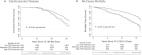
Pierce and colleagues used the CARDIA (Coronary Artery Risk Development in Young Adults)
study to perform a large longitudinal cohort study to evaluate the association between
childhood adversity and the long‐term development of CVD and the risk of death among
geographically and racially diverse participants (47% black).4 With over 30 years
of follow‐up, they found that self‐reported childhood adversity was associated with
an increased risk of death and CVD events. The study highlights that childhood is
a critical developmental period for the development of CVD and risk of death over
the lifespan. Of note, following adjustment for demographic, socioeconomic, clinical,
and psychological factors, the risk of CVD events was no longer significant, suggesting
that these factors are mediators of this relationship. The accompanying editorial
by Barr discusses education as perhaps the strongest mediator.5 Low education levels
are associated with higher rates of smoking, a present‐fatalistic perspective, and
social networks that affirm such behaviors and perspectives.
Stress and psychological factors may act through many different complex mechanisms.
One premise is that stress and adverse experiences predispose to behavioral risk factors,
such as smoking, substance use, poor diet, and sedentary lifestyle. Those with poor
psychosocial health may also have limited access to care and insurance. Physiologic
mechanisms are also at play and include abnormal inflammatory and neurohormonal processes.
Stress may also induce elevated blood pressure and glucose dysregulation. In this
issue, Greaney and colleagues add to the literature on the physiologic response to
stress.6 They found that among healthy young adults, psychosocial stress adversely
influenced microvascular vasoconstrictor function. Interestingly, this was regardless
of the severity or the emotional consequences of the stress. In addition, Yano and
colleagues found that sleep‐disordered breathing was associated with higher blood
glucose levels among blacks.7
Although stress may lead to increased morbidity and mortality from CVD, psychosocial
well‐being may be protective. Goldmann and colleagues found that among patients who
survived a stroke, the perception that they can protect themselves from having a stroke
was associated with greater blood pressure reduction at 1 year.8 Positive health beliefs
may reflect optimism and self‐efficacy. To the contrary, Miller and colleagues evaluated
youth who achieved upward socioeconomic mobility and found that improving financial
conditions was associated with improved psychological well‐being but worse cardiometabolic
health.9 This study highlights that psychological well‐being and cardiovascular health
are not always aligned.
Poor cardiovascular health and, in particular, experiencing a traumatic medical event
may lead to psychosocial distress. Pasadyn and colleagues found that, among patients
who survived an acute type A aortic dissection, nearly a quarter screened positive
for posttraumatic stress disorder, with 44% reporting feeling on guard, watchful,
or easily startled.10 Similarly, Johnson and colleagues evaluated mental health among
patients who experienced spontaneous coronary artery dissection and found significant
rates of depression, anxiety, and posttraumatic stress disorder.11 They also found
that emotional and social quality of life was better among those with higher resiliency.
These studies highlight the importance of screening patients with these conditions
to refer them for further treatment of mental health and suggest that resiliency may
be protective. Although less traumatic, patients with adult congenital heart disease
experience ongoing health issues, interactions with the healthcare system, and perhaps
short‐term medical events. Carazo and colleagues found that the prevalence of depression
was nearly 20% among patients with adult congenital heart disease and that depression
was associated with increased all‐cause mortality, hospitalization, and systemic inflammation.12
Those who were depressed had lower education, lower physical activity, and higher
substance use, again raising the possibility that behaviors and education may play
an important mediating role in outcomes.
Additional research is needed to better understand the complex associations between
psychosocial factors and cardiovascular health and whether these factors can be modified
to improve outcomes and reduce disparities. In this Spotlight, Shabatun and colleagues
report the rationale for the Morehouse‐Emory Center for Health Equity, a study designed
to identify factors that predispose blacks to either increased risk or resilience
from CVD.13 In addition to exploring neighborhood and environmental factors, they
plan to focus on personal factors, including psychosocial, socioeconomic, health behaviors
and beliefs, and stress and risk profiles, and their association with prevalent and
subclinical CVD. Their goal is to elucidate new strategies and key points for effective
interventions to improve CVD outcomes in black communities. As part of this work,
they plan to randomize participants to a behavioral mobile health plus health coach
or mobile health only intervention and follow up for improvement.
Psychosocial factors and cardiovascular health are closely tied. As such, it is important
to recognize psychosocial factors and these associations as we work to prevent CVD,
treat patients with known disease, and improve both psychosocial well‐being and cardiovascular
health for all. This group of articles adds to our understanding of the epidemiology
and underlying mechanisms between psychosocial health and cardiovascular health. Finally,
it is important to understand the extent to which psychosocial factors contribute
to disparities in cardiovascular health and evaluate interventions addressing psychosocial
factors with the goal of eliminating these disparities.
Disclosures
Dr Peterson receives grant funding from the National Heart, Lung, and Blood Institute
(R33HL143324‐02).
Related collections
Most cited references13

- Record: found
- Abstract: found
- Article: found
Analysis of Posttraumatic Stress Disorder, Depression, Anxiety, and Resiliency Within the Unique Population of Spontaneous Coronary Artery Dissection Survivors
Alexis Johnson, Sharonne N Hayes, Craig N. Sawchuk … (2020)
- Record: found
- Abstract: found
- Article: found
Association of Childhood Psychosocial Environment With 30‐Year Cardiovascular Disease Incidence and Mortality in Middle Age
Jacob Pierce, Kiarri N Kershaw, Catarina Kiefe … (2020)
- Record: found
- Abstract: found
- Article: found
Sleep Characteristics and Measures of Glucose Metabolism in Blacks: The Jackson Heart Study
Yuichiro Yano, Yan Gao, Dayna A. Johnson … (2020)