- Record: found
- Abstract: found
- Article: not found
Clinical review: Hemorrhagic shock
Read this article at
Abstract
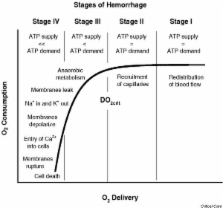
This review addresses the pathophysiology and treatment of hemorrhagic shock – a condition produced by rapid and significant loss of intravascular volume, which may lead sequentially to hemodynamic instability, decreases in oxygen delivery, decreased tissue perfusion, cellular hypoxia, organ damage, and death. Hemorrhagic shock can be rapidly fatal. The primary goals are to stop the bleeding and to restore circulating blood volume. Resuscitation may well depend on the estimated severity of hemorrhage. It now appears that patients with moderate hypotension from bleeding may benefit by delaying massive fluid resuscitation until they reach a definitive care facility. On the other hand, the use of intravenous fluids, crystalloids or colloids, and blood products can be life saving in those patients who are in severe hemorrhagic shock. The optimal method of resuscitation has not been clearly established. A hemoglobin level of 7–8 g/dl appears to be an appropriate threshold for transfusion in critically ill patients with no evidence of tissue hypoxia. However, maintaining a higher hemoglobin level of 10 g/dl is a reasonable goal in actively bleeding patients, the elderly, or individuals who are at risk for myocardial infarction. Moreover, hemoglobin concentration should not be the only therapeutic guide in actively bleeding patients. Instead, therapy should be aimed at restoring intravascular volume and adequate hemodynamic parameters.
Related collections
Most cited references69
- Record: found
- Abstract: found
- Article: not found
Immediate versus delayed fluid resuscitation for hypotensive patients with penetrating torso injuries.
- Record: found
- Abstract: found
- Article: not found
Human albumin administration in critically ill patients: systematic review of randomised controlled trials.
- Record: found
- Abstract: found
- Article: not found
