- Record: found
- Abstract: found
- Article: found
Social determinants of HIV infection, hotspot areas and subpopulation groups in Ethiopia: evidence from the National Demographic and Health Survey in 2011
Read this article at
Abstract
Objective
This study identifies social determinants of HIV infection, hotspot areas and subpopulation groups in Ethiopia.
Design
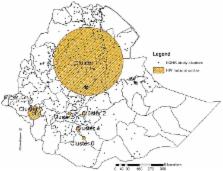
The study used data from the 2011 Ethiopian Demographic and Health Survey (EDHS). Sample blood tests from the finger pricks collected on filter paper cards were labelled with a barcode unique to each respondent. Spatial scan statistics and geographic information system tools were used to map hotspot areas of HIV prevalence. Bivariate and multivariable logistic regression models were used to identify social determinants of HIV infection.
Population
A total of 30 625 adults (16 515 women and 14 110 men) were included from 11 administrative states of Ethiopia.
Results
HIV prevalence reached 10–21% in the central, eastern and western geographic clusters of Ethiopia. Multivariable analysis showed that individuals who were in the middle, richer and richest wealth quintiles had increased odds of having HIV over those in the poorest quintile. Adults who had primary, secondary and higher educational levels had higher odds of being HIV positive than non-educated individuals. The odds of having HIV were higher among adults who had multiple lifetime sexual partners than those with a single partner. An increasing odds of HIV infection were observed among adults in the age groups of 25–29, 30–34, 35–39 and 40–45 years compared with adults in the age group of 45–49 years. Merchants had higher odds of being HIV positive than those who were not employed. The odds of having HIV were higher among urban residents and females than among rural residents and males, respectively.
Related collections
Most cited references30
- Record: found
- Abstract: found
- Article: found
Women and HIV in Sub-Saharan Africa
- Record: found
- Abstract: not found
- Article: not found