- Record: found
- Abstract: found
- Article: found
Comparison of the effects of ketamine and fentanyl-midazolam-medetomidine for sedation of rhesus macaques ( Macaca mulatta)
Read this article at
Abstract
Background
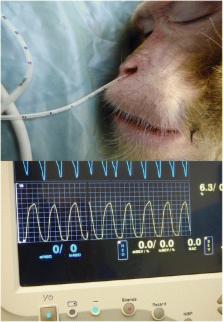
This study assessed the effects of sedation using a combination of fentanyl, midazolam and medetomidine in comparison to ketamine. Rhesus Macaques ( Macaca mulatta), ( n = 16, 5 males and 3 females randomly allocated to each treatment group) received either ketamine (KET) (10 mg.kg −1) or fentanyl-midazolam-medetomidine (FMM) (10 μg/kg −1; 0.5 mg.kg −1; 20 μg.kg −1) both IM. Oxygen (100 %) was provided by mask and heart rate, blood pressure, respiratory rate, EtCO 2 and depth of sedation were assessed every 5 min for 20 min. After the last time point, FMM monkeys were reversed with atipamezole-naloxone (0.2 mg.kg −1; 10 μg.kg −1). Recovery was scored using clinical scoring scheme. Differences in physiological parameters and quality of sedation were compared using Area Under the Curve (AUC) method and either Mann-Witney or t-student tests.
Results
Heart rate (beats/min) (Ket = 119 ± 18; FMM = 89 ± 17; p = 0.0066), systolic blood pressure (mmHg) (Ket = 109 ± 10; FMM = 97 ± 10; p = 0.0313), and respiratory rate (breaths/min) (Ket = 39 ± 9; FMM = 29 ± 10; p = 0.0416) were significantly lower in the FMM group. End-tidal CO 2 (mmHg) did not differ between the groups (KET = 33 ± 8; FMM = 42 ± 11; p = 0.0462) . Although some depression of physiological parameters was seen with FMM, the variables all remained within the normal ranges in both groups. Onset of a sufficient degree of sedation for safe handling was more rapid with ketamine (KET = 2.9 ± 1.4 min; FMM = 7.9 ± 1.2 min; p = 0.0009), but FMM recovery was faster (KET = 21.4 ± 13.4 min; FMM = 9.1 ± 3.6 min; p = 0.0379) and of better quality (KET = 1.3 ± 0.9; FMM = 7.4 ± 1.9; p = 0.0009) most probably because of the effectiveness of the reversal agents used.
Related collections
Most cited references48
- Record: found
- Abstract: found
- Article: not found
Development and psychometric evaluation of the pediatric anesthesia emergence delirium scale.
- Record: found
- Abstract: found
- Article: not found
Incidence, Reversal, and Prevention of Opioid-induced Respiratory Depression.
- Record: found
- Abstract: found
- Article: not found