- Record: found
- Abstract: found
- Article: found
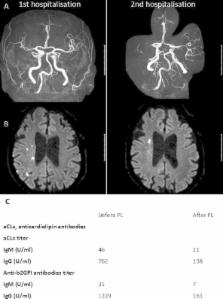
Rapidly progressive intracranial artery stenosis in primary antiphospholipid syndrome
Read this article at
Abstract
Antiphospholipid antibody syndrome (APS) is usually a disease of young adults. In elderly stroke patients APS was not associated with progressive intracerebral stenosis in the past. Here, we report a 65-year-old patient who presented with recurrent ischemic strokes associated with progressive stenosis of the right middle cerebral artery. Antiphospholipid antibodies were detected and treatment with plasma exchange, tapered steroids, and anticoagulants was successful. This case demonstrates that APS should be considered also in elderly stroke patients. This is of particular relevance since APS confers a significant risk to angioplasty and stenting procedures which therefore should be avoided in APS.
Related collections
Most cited references11
- Record: found
- Abstract: found
- Article: not found
Stenting versus aggressive medical therapy for intracranial arterial stenosis.
- Record: found
- Abstract: found
- Article: not found