- Record: found
- Abstract: found
- Article: found
Assessing small airway disease in GLI versus NHANES III based spirometry using area under the expiratory flow-volume curve
Read this article at
Abstract
Background
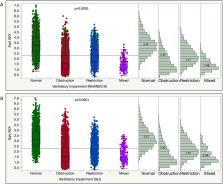
Spirometry interpretation is influenced by the predictive equations defining lower limit of normal (LLN), while ‘distal’ expiratory flows such as forced expiratory flow at 50% FVC (FEF 50) are important functional parameters for diagnosing small airway disease (SAD). Area under expiratory flow-volume curve (AEX) or its approximations have been proposed as supplemental spirometric assessment tools. We compare here the performance of AEX in differentiating between normal, obstruction, restriction, mixed defects and SAD, as defined by Global Lung Initiative (GLI) or National Health and Nutrition Examination Survey (NHANES) III reference values, and using various predictive equations for FEF 50.
Methods
We analysed 15 308 spirometry-lung volume tests. Using GLI versus NHANES III LLNs, and diagnosing SAD by the eight most common equation sets for forced expiratory flow at 50% of vital capacity lower limits of normal (FEF 50 LLN), we assessed the degree of diagnostic concordance and the ability of AEX to differentiate between various definition-dependent patterns.
Results
Concordance rates between NHANES III and GLI-based classifications were 93.7%, 78.6%, 86.8%, 88.0%, 93.8% and 98.8% in those without, with mild, moderate, moderately severe, severe and very severe obstruction, respectively (agreement coefficient 0.81 (0.80–0.82)). The prevalence of SAD was 0.6%–6.9% of the cohort, depending on the definition used. The AEX differentiated well between normal, obstruction, restriction, mixed pattern and SAD, as defined by most equations.
Conclusions
If the SAD diagnosis is established by using mean FEF 50 LLN or a set number of predictive equations, AEX is able to differentiate well between various spirometric patterns. Using the most common predictive equations (NHANES III and GLI), the diagnostic concordance for functional type and obstruction severity is high.
Related collections
Most cited references25
- Record: found
- Abstract: not found
- Article: not found
Lung function testing: selection of reference values and interpretative strategies. American Thoracic Society.
- Record: found
- Abstract: found
- Article: not found
Impulse oscillometry: interpretation and practical applications.
- Record: found
- Abstract: found
- Article: not found