- Record: found
- Abstract: found
- Article: found
Under Utilization of local anesthetics in infant lumbar punctures
Read this article at
Abstract
Background
Lumbar Puncture (LP) is an invasive procedure frequently used to diagnose meningitis among the pediatric population. Neonates and infants have not routinely received local anesthesia prior to LP.
Study Objective
To determine whether emergency medicine physicians and pediatricians use local analgesics on neonates and infants prior to performing an LP and to identify which local anesthetics, if any, were used.
Methods
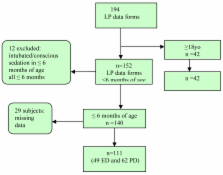
Prospective, cohort study of all infants, six months of age or less, that received an LP in the emergency department (ED) or inpatient pediatric units for suspected meningitis during a period of year at a university tertiary care hospital.
Results
A total sample population of 111 infants that received an LP within the study period. A control population of 42 adults received an LP. Only 40.4% (45/111) of the infants received local analgesia prior to LP: either 1% lidocaine, EMLA or a combination of the two. Infants were less likely to receive lidocaine or EMLA prior to LP compared to adult subjects (OR= 0.27; 95% CI0.12 to 0.62). No neonates that were less than one month of age received local procedural anesthesia by emergency medicine or pediatric physicians. ED physicians’ use of local anesthesia prior to LP increased with increasing age of the infant. The pediatricians in this study used local anesthesia prior to LP when the infant was at least five months of age.
Related collections
Most cited references9
- Record: found
- Abstract: found
- Article: not found
Consequences of inadequate analgesia during painful procedures in children.
- Record: found
- Abstract: found
- Article: not found
Local anesthetic and stylet styles: factors associated with resident lumbar puncture success.
- Record: found
- Abstract: found
- Article: not found