- Record: found
- Abstract: found
- Article: found
Growth hormone deficiency, secondary hypothyroidism, and empty sella following treatment of childhood macroprolactinoma
Read this article at
Abstract
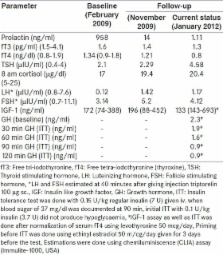
Macroprolactinoma are rare in childhood, especially in the first decade. A 9-year-old girl presented with headache, vomiting, and decreased vision for 8 months. A diagnosis of macroprolactinoma was made following documentation of elevated serum prolactin (958 ng/ml) with a contrast enhancing macroadenoma (30 × 27 × 28 mm) on magnetic resonance imaging of pituitary. Anterior pituitary function was normal. Cabergoline therapy resulted in resolution of all symptoms in 2-8 months. Revaluation at 10 months of cabergoline therapy revealed normal serum prolactin (14 ng/ml), normal pituitary function, with 91% decrease in adenoma size (11.5 × 13.6 × 12.7 mm). Evaluation at 36 months of cabergoline therapy for growth arrest and weight gain for past 6 months revealed low serum prolactin, growth hormone deficiency, and secondary hypothyroidism with empty sella. She had biochemical as well as structural resolution of prolactinoma. This report highlights the development of multiple pituitary hormone deficiency with empty sella, an uncommon side effect of cabergoline therapy for macroprolactinoma.
Related collections
Most cited references8
- Record: found
- Abstract: found
- Article: not found
A comparison of cabergoline and bromocriptine in the treatment of hyperprolactinemic amenorrhea. Cabergoline Comparative Study Group.
- Record: found
- Abstract: found
- Article: not found
Long-term remission following withdrawal of dopamine agonist therapy in subjects with microprolactinomas.
- Record: found
- Abstract: found
- Article: not found