- Record: found
- Abstract: found
- Article: not found
Volunteer patients and small groups contribute to abdominal examination’s success
Read this article at
Abstract
Background
Prior to 2007, we taught the abdominal examination in a hospital based group to 40 students, at one hospital. We used volunteer patients, small groups, repetition, and required faculty development sessions. In 2007, our medical school changed its “Introduction to Physical Examination” session so that the entire class was to be taught in a geographically central session. Our hospital was selected to lead the abdominal examination portion of the session.
Aim
Our aim was to answer three questions. First, could we quadruple the recruitment of volunteer patients, and faculty? Second, was it volunteer patients, small groups, repetition, or faculty training that was most valued by the students? Third, would volunteer patients and/or faculty agree to participate a second time?
Methods
A total of 43–46 patients and 43–46 faculty were recruited and 43–46 examining rooms were obtained for each of the 5 years of this study. Teachers were required to attend a 1-hour faculty development session. The class of about 170 students was divided into 43–46 groups each year. The teacher demonstrated the abdominal examination and each student practiced the examination on another student. Each student then repeated the full abdominal examination on a volunteer patient.
Results
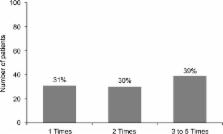
Over the 5-year time period (2008–2012), the abdominal examination ranked first among all organ systems’ “Introductory Sessions”. The abdominal examination ratings had the best mean score (1.35) on a Likert scale where 1 is excellent and 5 is poor. The students gave the most positive spontaneous comments to having volunteer patients, with small groups coming in as the second most appreciated educational element.
Conclusion
We successfully quadrupled the number of faculty, patients, and examining rooms and created a highly rated educational program as measured by anonymous student evaluations, patient and faculty participation, and the medical school’s selecting the abdominal examination methods as an “Advanced Examination” for the Pathways Curriculum.
Related collections
Most cited references31
- Record: found
- Abstract: found
- Article: not found
Effects of basic clinical skills training on objective structured clinical examination performance.
- Record: found
- Abstract: found
- Article: not found
Does ultrasound training boost Year 1 medical student competence and confidence when learning abdominal examination?
- Record: found
- Abstract: found
- Article: not found
