- Record: found
- Abstract: found
- Article: found
Hospital level variations in the trends and outcomes of the nonoperative management of splenic injuries – a nationwide cohort study
Read this article at
Abstract
Background
The long-term treatment trends of splenic injuries can provide guidance when treating trauma patients. The nonoperative management (NOM) of splenic injuries was introduced in early 1989. After decades of development, it has proven to be safe and is now the primary treatment choice worldwide. However, there remains a lack of nationwide registry data to support the feasibility and efficiency of NOM.
Methods
We used the Taiwan National Health Insurance Research Database to conduct a whole population-based cohort study. Patients admitted with blunt splenic injuries from 2002 to 2013 were identified. Demographic data, management methods, associated injuries, comorbidities and outcome parameters were collected. Patients were divided into 2 groups by the type of admitting institution: a tertiary center or a non-center hospital. We also used 4 years as an interval to analyze the changes in epidemiological data and treatment trends. Comparisons of the results of NOM and surgical management were also performed.
Results
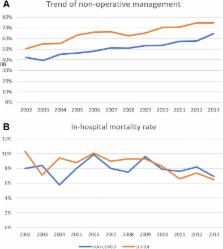
A total of 12,455 patients were admitted with blunt splenic injuries between 2002 and 2013. Among the 11,551 patients treated in a single hospital after admission, patients underwent NOM more frequently at tertiary centers than at non-center hospitals (64.6% vs 50.3%). During the 12-year study period, the NOM rate increased from 56 to 73% in tertiary centers, while in noncenter hospitals, the rate only increased from 43 to 58%. The mortality rate decreased in tertiary centers from 8.9 to 7.2%, with no apparent change in noncenter hospitals. Complications occurred more frequently in the surgical management group.
Related collections
Most cited references23
- Record: found
- Abstract: found
- Article: not found
Selective nonoperative management of blunt splenic injury: an Eastern Association for the Surgery of Trauma practice management guideline.
- Record: found
- Abstract: found
- Article: not found
Nonoperative management of blunt splenic injury: a 5-year experience.
- Record: found
- Abstract: found
- Article: not found