- Record: found
- Abstract: found
- Article: found
National Institutes of Health–Funded Cardiac Arrest Research: A 10‐Year Trend Analysis
Read this article at
Abstract
Background
Cardiac arrest ( CA) is a leading cause of death in the United States, claiming over 450 000 lives annually. Improving survival depends on the ability to conduct CA research and on the translation and implementation of research findings into practice. Our objective was to provide a descriptive analysis of annual National Institutes of Health ( NIH) funding for CA research over the past decade.
Method and Results
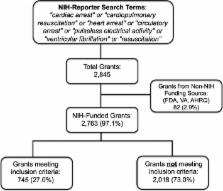
A search within NIH Re PORTER for the years 2007 to 2016 was performed using the terms: “cardiac arrest” or “cardiopulmonary resuscitation” or “heart arrest” or “circulatory arrest” or “pulseless electrical activity” or “ventricular fibrillation” or “resuscitation.” Grants were reviewed and categorized as CA research (yes/no) using predefined criteria. The annual NIH funding for CA research, number of individual grants, and principal investigators were tabulated. The total NIH investment in CA research for 2015 was calculated and compared to those for other leading causes of death within the United States. Interrater reliability among 3 independent reviewers for fiscal year 2015 was assessed using Fleiss κ. The search yielded 2763 NIH‐funded grants, of which 745 (27.0%) were classified as CA research (κ=0.86 [95% CI 0.80‐0.93]). Total inflation‐adjusted NIH funding for CA research was $35.4 million in 2007, peaked at $76.7 million in 2010, and has decreased to $28.5 million in 2016. Per annual death, NIH invests ≈$2200 for stroke, ≈$2100 for heart disease, and ≈$91 for CA.
Related collections
Most cited references5
- Record: found
- Abstract: found
- Article: not found
Incidence of treated cardiac arrest in hospitalized patients in the United States.
- Record: found
- Abstract: found
- Article: not found
Cardiac arrest: a public health perspective.
- Record: found
- Abstract: not found
- Article: not found