- Record: found
- Abstract: found
- Article: found
Systemic lycopene as an adjunct to scaling and root planing in chronic periodontitis patients with type 2 diabetes mellitus
Read this article at
Abstract
Background:
Patients with type 2 diabetes have an increased prevalence of periodontitis and, in turn, periodontitis adversely affects the diabetic status. Oxidative stress plays a key role in affecting the pathophysiology of both the diseases and adjunctive systemic antioxidant therapy may have beneficial effect on the treatment outcome. This study was planned to compare the efficacy of systemic antioxidant therapy with lycopene as an adjunct to scaling and root planing versus scaling and root planing alone in chronic periodontitis patients with type 2 diabetes mellitus.
Materials and Methods:
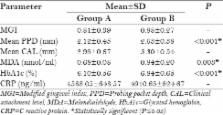
40 diabetic subjects with periodontitis, attending the OP wing of the Department of Periodontics of a tertiary referral care hospital were randomized and equally divided into group A and group B. Diabetes status was recorded as per ADA guidelines and the periodontitis status as per American Academy of Periodontology (AAP) guidelines. Group A patients underwent scaling and root planing with administration of lycopene 8 mg and group B patients were treated with scaling and root planing alone. Clinical parameters like gingival index (GI), probing depth (PD), and clinical attachment level (CAL) were recorded. Serum markers, i.e. malondialdehyde (MDA) (TBARS assay) and C reactive protein (CRP) (ELISA), and glycated hemoglobin (HbA1c) levels were assessed at baseline and at 2 months and 6 months post-therapy.
Related collections
Most cited references30
- Record: found
- Abstract: found
- Article: not found
Malondialdehyde and thiobarbituric acid-reactivity as diagnostic indices of lipid peroxidation and peroxidative tissue injury.
- Record: found
- Abstract: not found
- Article: not found
The role of reactive oxygen and antioxidant species in periodontal tissue destruction.
- Record: found
- Abstract: not found
- Article: not found