- Record: found
- Abstract: found
- Article: found
Interfraction variation and dosimetric changes during image-guided radiation therapy in prostate cancer patients
Read this article at
Abstract
Purpose
The aim of this study was to identify volume changes and dose variations of rectum and bladder during radiation therapy in prostate cancer (PC) patients.
Materials and Methods
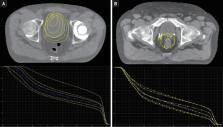
We analyzed 20 patients with PC treated with helical tomotherapy. Daily image guidance was performed. We re-contoured the entire bladder and rectum including its contents as well as the organ walls on megavoltage computed tomography once a week. Dose variations were analyzed by means of Dmedian, Dmean, Dmax, V 10 to V 75, as well as the organs at risk (OAR) volume. Further, we investigated the correlation between volume changes and changes in Dmean of OAR.
Results
During treatment, the rectal volume ranged from 62% to 223% of its initial volume, the bladder volume from 22% to 375%. The average Dmean ranged from 87% to 118% for the rectum and 58% to 160% for the bladder. The Pearson correlation coefficients between volume changes and corresponding changes in Dmean were -0.82 for the bladder and 0.52 for the rectum. The comparison of the dose wall histogram (DWH) and the dose volume histogram (DVH) showed that the DVH underestimates the percentage of the rectal and bladder volume exposed to the high dose region.
Conclusion
Relevant variations in the volume of OAR and corresponding dose variations can be observed. For the bladder, an increase in the volume generally leads to lower doses; for the rectum, the correlation is weaker. Having demonstrated remarkable differences in the dose distribution of the DWH and the DVH, the use of DWHs should be considered.
Related collections
Most cited references19
- Record: found
- Abstract: found
- Article: not found
Improved clinical outcomes with high-dose image guided radiotherapy compared with non-IGRT for the treatment of clinically localized prostate cancer.
- Record: found
- Abstract: found
- Article: not found
Organ motion and its management.
- Record: found
- Abstract: found
- Article: not found