- Record: found
- Abstract: found
- Article: found
Anti-Epileptic Effects of FABP3 Ligand MF1 through the Benzodiazepine Recognition Site of the GABA A Receptor
Read this article at
Abstract
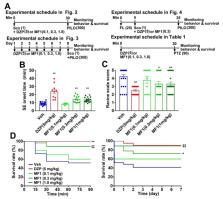
Recently, we developed the fatty acid-binding protein 3 (FABP3) ligand MF1 (4-(2-(1-(2-chlorophenyl)-5-phenyl-1H-pyrazol-3-yl)phenoxy) butanoic acid) as a therapeutic candidate for α-synucleinopathies. MF1 shows affinity towards γ-aminobutyric acid type-A (GABA A) receptor, but its effect on the receptor remains unclear. Here, we investigate the pharmacological properties of MF1 on the GABA A receptor overexpressed in Neuro2A cells. While MF1 (1–100 μm) alone failed to evoke GABA currents, MF1 (1 μm) promoted GABA currents during GABA exposure (1 and 10 μm). MF1-promoted GABA currents were blocked by flumazenil (10 μm) treatment, suggesting that MF1 enhances receptor function via the benzodiazepine recognition site. Acute and chronic administration of MF1 (0.1, 0.3 and 1.0 mg/kg, p.o.) significantly attenuated status epilepticus (SE) and the mortality rate in pilocarpine (PILO: 300 mg/kg, i.p.)-treated mice, similar to diazepam (DZP: 5.0 mg/kg, i.p.). The anti-epileptic effects of DZP (5.0 mg/kg, i.p.) and MF1 (0.3 mg/kg, p.o.) were completely abolished by flumazenil (25 mg/kg, i.p.) treatment. Pentylenetetrazol (PTZ: 90 mg/kg, i.p.)-induced seizures in mice were suppressed by DZP (5.0 mg/kg, i.p.), but not MF1. Collectively, this suggests that MF1 is a mild enhancer of the GABA A receptor and exercises anti-epileptic effects through the receptor’s benzodiazepine recognition site in PILO-induced SE models.
Related collections
Most cited references42
- Record: found
- Abstract: found
- Article: not found
Animal Models of Seizures and Epilepsy: Past, Present, and Future Role for the Discovery of Antiseizure Drugs
- Record: found
- Abstract: found
- Article: not found
Benzodiazepines in epilepsy: pharmacology and pharmacokinetics.
- Record: found
- Abstract: found
- Article: found