- Record: found
- Abstract: found
- Article: found
Arrhythmic risk stratification in post-myocardial infarction patients with preserved ejection fraction: the PRESERVE EF study
Read this article at
Abstract
Aims
Sudden cardiac death (SCD) annual incidence is 0.6–1% in post-myocardial infarction (MI) patients with left ventricular ejection fraction (LVEF)≥40%. No recommendations for implantable cardioverter-defibrillator (ICD) use exist in this population.
Methods and results
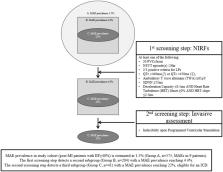
We introduced a combined non-invasive/invasive risk stratification approach in post-MI ischaemia-free patients, with LVEF ≥ 40%, in a multicentre, prospective, observational cohort study. Patients with at least one positive electrocardiographic non-invasive risk factor (NIRF): premature ventricular complexes, non-sustained ventricular tachycardia, late potentials, prolonged QTc, increased T-wave alternans, reduced heart rate variability, abnormal deceleration capacity with abnormal turbulence, were referred for programmed ventricular stimulation (PVS), with ICDs offered to those inducible. The primary endpoint was the occurrence of a major arrhythmic event (MAE), namely sustained ventricular tachycardia/fibrillation, appropriate ICD activation or SCD. We screened and included 575 consecutive patients (mean age 57 years, LVEF 50.8%). Of them, 204 (35.5%) had at least one positive NIRF. Forty-one of 152 patients undergoing PVS (27–7.1% of total sample) were inducible. Thirty-seven (90.2%) of them received an ICD. Mean follow-up was 32 months and no SCDs were observed, while 9 ICDs (1.57% of total screened population) were appropriately activated. None patient without NIRFs or with NIRFs but negative PVS met the primary endpoint. The algorithm yielded the following: sensitivity 100%, specificity 93.8%, positive predictive value 22%, and negative predictive value 100%.
Related collections
Most cited references31
- Record: found
- Abstract: not found
- Article: not found
2017 AHA/ACC/HRS Guideline for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society
- Record: found
- Abstract: found
- Article: not found
Prophylactic use of an implantable cardioverter-defibrillator after acute myocardial infarction.
- Record: found
- Abstract: found
- Article: not found
