Journal ID (nlm-ta): Mov Disord
Journal ID (iso-abbrev): Mov Disord
Journal ID (doi): 10.1002/(ISSN)1531-8257
Journal ID (publisher-id): MDS
Title:
Movement Disorders
Publisher:
John Wiley & Sons, Inc.
(Hoboken, USA
)
ISSN
(Print):
0885-3185
ISSN
(Electronic):
1531-8257
Publication date
(Electronic):
20
October
2020
Publication date
(Print):
February
2021
Volume: 36
Issue: 2
(
doiID:
10.1002/mds.v36.2
)
Pages: 503-508
Affiliations
[
1
]
Department of Clinical and Movement Neurosciences
Reta Lila Weston Institute, UCL Queen Square Institute of Neurology
London
United Kingdom
[
2
]
Dementia Research Centre, Department of Neurodegenerative Disease
UCL Queen Square Institute of Neurology
London
United Kingdom
[
3
]
Department of Neurodegenerative Disease
UK Dementia Research Institute, UCL Queen Square Institute of Neurology
London
United Kingdom
[
4
]
Department of Clinical Chemistry
Northern General Hospital
Sheffield
United Kingdom
[
5
]
UCL Institute for Liver and Digestive Health
Royal Free Hospital and UCL
London
United Kingdom
[
6
]
Department of Clinical Neurosciences
University of Cambridge and Cambridge University Hospitals Trust
Cambridge
United Kingdom
[
7
]
Division of Neuroscience and Experimental Psychology, Wolfson Molecular Imaging Centre
University of Manchester
Manchester
United Kingdom
[
8
]
Departments of Geriatric Medicine and Nuclear Medicine
University of Duisburg‐Essen
Duisburg
Germany
[
9
]
Department of Brain Sciences
Imperial College London
London
United Kingdom
[
10
]
Nuffield Department of Clinical Neurosciences
University of Oxford
Oxford
United Kingdom
[
11
]
Departamento de Neurología
Pontificia Universidad Católica de Chile
Santiago
Chile
[
12
]
Sunnybrook Health Sciences Centre
Sunnybrook Research Institute, University of Toronto
Toronto
Ontario
Canada
[
13
]
Neuro‐Ophthalmology
National Hospital for Neurology and Neurosurgery
London
United Kingdom
[
14
]
Department of Clinical Biochemistry
Southampton General Hospital
Southampton
United Kingdom
[
15
]
Clinical Neurochemistry Laboratory
Sahlgrenska University Hospital
Mölndal
Sweden
[
16
]
Department of Psychiatry and Neurochemistry
Institute of Neuroscience and Physiology, the Sahlgrenska Academy at the University
of Gothenburg
Mölndal
Sweden
[
17
]
Sheffield Institute for Translational Neuroscience, University of Sheffield
Sheffield
United Kingdom
Author notes
[*]
[*
]
Correspondence to: Dr. Thomas T. Warner, Reta Lila Weston Institute, 1 Wakefield Street, London WCN1
1PJ, United Kingdom; E‐mail:
t.warner@
123456ucl.ac.uk
Author information
Article
Publisher ID:
MDS28333
DOI: 10.1002/mds.28333
PMC ID: 8436757
PubMed ID: 33078859
SO-VID: bc929205-c812-400f-a215-87ba2e019075
Copyright © © 2020 University College London.
Movement Disorders published by Wiley Periodicals LLC on behalf of International Parkinson and Movement
Disorder Society
License:
This is an open access article under the terms of the
http://creativecommons.org/licenses/by/4.0/ License, which permits use, distribution and reproduction in any medium, provided
the original work is properly cited.
Page count
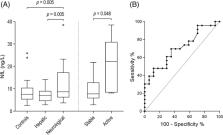
Figures: 1,
Tables: 1,
Pages: 5,
Words: 3828
Funded by: Association of British Neurologists
Funded by: Canadian Institutes of Health Research
, doi 10.13039/501100000024;
Funded by: European Research Council
, doi 10.13039/100010663;
Funded by: Guarantors of Brain
, doi 10.13039/501100000627;
Funded by: Reta Lila Weston Institute
Funded by: Wellcome Trust
, doi 10.13039/100010269;
Funded by: Wilson's Disease Support Group UK