- Record: found
- Abstract: found
- Article: found
Intrapartum and neonatal mortality among low-risk women in midwife-led versus obstetrician-led care in the Amsterdam region of the Netherlands: a propensity score matched study
Read this article at
Abstract
Objective
To compare intrapartum and neonatal mortality in low-risk term women starting labour in midwife-led versus obstetrician-led care.
Study design
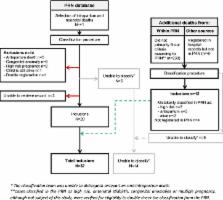
We performed a propensity score matched study using data from our national perinatal register, completed with data from medical files. We studied women without major risk factors with singleton pregnancies who gave birth at term between 2005 and 2008 in the Amsterdam region of the Netherlands. Major risk factors comprised non-vertex position of the fetus, previous Caesarean birth, hypertension, (gestational) diabetes mellitus, post-term pregnancy (≥42 weeks), prolonged rupture of membranes (>24 hours), vaginal bleeding in the second half of pregnancy or induced labour. Groups were devided by midwife-led versus obstetrician-led care at the onset of labour. The primary outcome was intrapartum and neonatal (<28 days) mortality. Secondary outcomes included obstetric interventions, 5 min Apgar scores<7 and neonatal intensive care admittance for >24 hours.
Results
We studied 57 396 women. Perinatal mortality occurred in 30 of 46 764 (0.64‰) women in midwife-led care and in 2 of 10 632 (0.19‰) women in obstetrician-led care (OR 3.4, 95% CI 0.82 to 14.3). A propensity score matched analysis in a 1:1 ratio with 10 632 women per group revealed an OR for perinatal mortality of 4.0 (95% CI 0.85 to 18.9).
Related collections
Most cited references19
- Record: found
- Abstract: not found
- Article: not found
Scientific method: statistical errors.
- Record: found
- Abstract: found
- Article: not found
Methods for constructing and assessing propensity scores.
- Record: found
- Abstract: found
- Article: not found