- Record: found
- Abstract: found
- Article: found
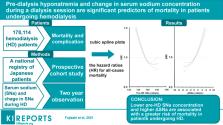
Pre-dialysis Hyponatremia and Change in Serum Sodium Concentration During a Dialysis Session Are Significant Predictors of Mortality in Patients Undergoing Hemodialysis
Read this article at
Abstract
Background
Previous studies have shown that hyponatremia is associated with greater mortality in hemodialysis (HD) patients. However, there have been few reports regarding the importance of the change in serum sodium (SNa) concentration (ΔSNa) during dialysis sessions. To investigate the relationships of pre-dialysis hyponatremia and ΔSNa during a dialysis session with mortality, we analyzed data from a national registry of Japanese patients with end-stage kidney disease.
Methods
We identified 178,114 patients in the database who were undergoing HD 3 times weekly. The study outcome was 2-year all-cause mortality, and the baseline SNa concentrations were categorized into quintiles. We evaluated the relationships of SNa concentration and ΔSNa with mortality using Cox proportional hazards models.
Results
During a 2-year follow-up period, 25,928 patients died. Each 1-mEq/l reduction in pre-HD SNa concentration was associated with a cumulatively greater risk of all-cause mortality (hazard ratio [HR], 1.05; 95% confidence interval [CI], 1.05–1.06). In contrast, a larger ΔSNa was associated with higher all-cause mortality (HR for a 1-mEq/l increase in ΔSNa, 1.02; 95% CI 1.01–1.02). The combination of low pre-HD SNa concentration and large ΔSNa was also associated with higher mortality (HR 1.09; 95% CI 1.05–1.13). Participants with the lowest SNa concentration (≤136 mEq/L) and the highest ΔSNa (>4 mEq/L) showed higher mortality than those with an intermediate pre-HD SNa concentration (137–140 mEq/L) and the lowest ΔSNa (≤2 mEq/L).
Graphical abstract
Related collections
Most cited references26
- Record: found
- Abstract: found
- Article: not found
Relationship between admission serum sodium concentration and clinical outcomes in patients hospitalized for heart failure: an analysis from the OPTIMIZE-HF registry.
- Record: found
- Abstract: found
- Article: not found
Hyponatremia and mortality: moving beyond associations.
- Record: found
- Abstract: found
- Article: found
