- Record: found
- Abstract: found
- Article: found
Platelet-Rich Plasma for Sport-Active Patients with Knee Osteoarthritis: Limited Return to Sport
Read this article at
Abstract
Objective
To evaluate a cohort of sport-active patients suffering from cartilage degeneration and OA, in terms of clinical outcome and return to sport (RTS) after platelet-rich plasma (PRP) injective treatment.
Design
This study included forty-seven sport-active patients ≤50 years old with unilateral symptomatic knee cartilage degeneration or OA. Patients received 3 PRP injections and were prospectively evaluated at baseline and then at 2, 6, 12, and 24 months follow-up by IKDC subjective EQ-VAS, and Tegner scores. Furthermore, patients were asked about their RTS, in terms of return to any sport level or to their activity level before symptoms onset.
Results
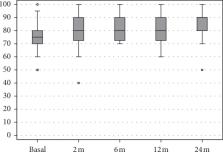
IKDC subjective score improved significantly at all follow-ups, changing from 59.2 ± 13.6 to 70.6 ± 13 at 12 months and to 76.7 ± 12.5 at 24 months ( p < 0.0005). A similar outcome was observed with the EQ-VAS score. Tegner score improved from 3.6 ± 1.4 to 4.8 ± 0.9 at 24 months ( p < 0.0005). A similar outcome was observed with the EQ-VAS score. Tegner score improved from 3.6 ± 1.4 to 4.8 ± 0.9 at 24 months ( p < 0.0005). A similar outcome was observed with the EQ-VAS score. Tegner score improved from 3.6 ± 1.4 to 4.8 ± 0.9 at 24 months ( p < 0.0005). A similar outcome was observed with the EQ-VAS score. Tegner score improved from 3.6 ± 1.4 to 4.8 ± 0.9 at 24 months (
Conclusions
Sport-active patients affected by knee OA can benefit from PRP injections, with pain and function improvement over time. However, results are less satisfactory in terms of RTS since only half can achieve the same sport level as before the onset of symptoms. Patients undergoing PRP treatment should be made aware of their low chances to go back to high-impact sport activities.
Related collections
Most cited references31
- Record: found
- Abstract: found
- Article: not found
Risk factors for the incidence and progression of radiographic knee osteoarthritis.
- Record: found
- Abstract: found
- Article: not found
Patient satisfaction after knee arthroplasty: a report on 27,372 knees operated on between 1981 and 1995 in Sweden.
- Record: found
- Abstract: found
- Article: not found