- Record: found
- Abstract: found
- Article: found
PAEDIATRIC ENDOCRINE DISORDERS AT THE UNIVERSITY COLLEGE HOSPITAL, IBADAN: 2002 – 2009
Read this article at
Abstract
Background:
Until recently, most published research focus more on infectious diseases and malnutrition giving the impression that endocrine disorders are uncommon. Reports on endocrine disorders in children in developing countries are few compared to developed countries reflecting the different level of prevalence in the different geographical locations and or level of awareness and availability of facilities for proper diagnosis.
Subjects/Methods:
A review of records of children who presented at University College Hospital, Ibadan with paediatric endocrine disorders from 2002 to 2009 was carried out.
Results:
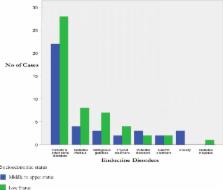
During the eight-year period, a total of 110 children presented with various endocrine disorders but only 94 had complete data for this study. There were 47(50%) males and 37(39.4%) females, and in 10(10.6%) of them, had genital ambiguity at presentation. Patients’ ages ranged from 2 weeks to 15 years with a median of 3 years. Many (35%) patients were malnourished with weight less than 80% of the expected weight for age and only 9% were overweight. Yearly distribution of cases showed a steady increase in number of cases from 2005. Rickets and metabolic disorders constituted 56.4% of patients; Diabetes mellitus was diagnosed in 12.8%, adrenal disoders in 10.6%, pubertal disorders in 5.3% and growth disorders in 4.3% of the patients. Thyroid disorders were present in 6.4%, obesity in 3.2% while the least common disorder was Diabetes insipidus (1%). About 58% of the children had parents in the low socioeconomic status and the management of the cases were severely hampered by lack of funds. About 60.6% of these patients were lost to follow up, during the period.
Related collections
Most cited references11
- Record: found
- Abstract: found
- Article: not found
Maternal and fetal hypothalamic-pituitary-adrenal axes during pregnancy and postpartum.
- Record: found
- Abstract: found
- Article: not found
Prevalence of the metabolic syndrome among U.S. adolescents using the definition from the International Diabetes Federation.
- Record: found
- Abstract: found
- Article: not found