- Record: found
- Abstract: found
- Article: not found
Extracellular histones are major mediators of death in sepsis
Abstract
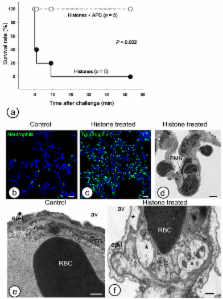
Hyper–inflammatory responses can lead to a variety of diseases including sepsis 1. We now report that extracellular histones released in response to inflammatory challenge contribute to endothelial dysfunction, organ failure and death during sepsis. They can be targeted pharmacologically by antibody to histone or by activated protein C (APC). Antibody to histone reduced the mortality of mice in lipopolysaccharide (LPS), tumor necrosis factor (TNF) or cecal ligation and puncture models of sepsis. Extracellular histones are cytotoxic toward endothelium in vitro and are lethal in mice. In vivo, histone administration resulted in neutrophil margination, vacuolated endothelium, intra–alveolar hemorrhage and macro and microvascular thrombosis. Histone was detected in the circulation of baboons challenged with E. coli and the increase in histone levels accompanied the onset of renal dysfunction. APC cleaves histones and reduces their cytotoxicity. Co–infusion of APC with E. coli in baboons or histones in mice prevented lethality. Blockade of protein C activation exacerbated sublethal LPS challenge into lethality which was reversed by antibody to histone. We conclude that extracellular histones are potential molecular targets for therapeutics for sepsis and other inflammatory diseases.
Related collections
Most cited references19
- Record: found
- Abstract: found
- Article: not found
Platelet TLR4 activates neutrophil extracellular traps to ensnare bacteria in septic blood.
- Record: found
- Abstract: found
- Article: not found
HMG-1 as a late mediator of endotoxin lethality in mice.
- Record: found
- Abstract: found
- Article: not found
